The Unique Occupational Environment of the Home Healthcare Worker
Posted on by Patient care is expanding beyond the walls of healthcare organizations. Improvements in technology, progression of disease management, and a growing number of persons seeking care within their homes are driving the growth of the home healthcare industry. Home healthcare workers (HHCWs) are a vital part of the rapidly growing industry and their work environment and occupational hazards are as diverse as the communities and homes they enter to provide care. The home healthcare service industry is one of the fastest growing industries. The U.S. Bureau of Labor Statistics ([BLS], 2020) reported the home health care service industry employed 1,527,400 workers in 2019 and is projected to increase by 29.9% to 1,983,400 by 2029. The workforce is made up of home care aides, registered nurses, physical, respiratory, and occupational therapists. The population of home healthcare aides is diverse, with 63% reporting to be persons of color in a workforce that is primarily female, and 52% of workers are over the age of 45 (PHI, 2019). HHCWs can be directly hired by the client or may work for a home healthcare agency and assigned to specific homes.
Patient care is expanding beyond the walls of healthcare organizations. Improvements in technology, progression of disease management, and a growing number of persons seeking care within their homes are driving the growth of the home healthcare industry. Home healthcare workers (HHCWs) are a vital part of the rapidly growing industry and their work environment and occupational hazards are as diverse as the communities and homes they enter to provide care. The home healthcare service industry is one of the fastest growing industries. The U.S. Bureau of Labor Statistics ([BLS], 2020) reported the home health care service industry employed 1,527,400 workers in 2019 and is projected to increase by 29.9% to 1,983,400 by 2029. The workforce is made up of home care aides, registered nurses, physical, respiratory, and occupational therapists. The population of home healthcare aides is diverse, with 63% reporting to be persons of color in a workforce that is primarily female, and 52% of workers are over the age of 45 (PHI, 2019). HHCWs can be directly hired by the client or may work for a home healthcare agency and assigned to specific homes.
Home Healthcare Workers
There are two types of workers who enter the home to provide care. The term “home health care” worker is defined as those who provide skilled, medical, clinical care in the home such as home health aides, occupational or physical therapists, nurses, speech therapists, and medical-social workers (Institute for Healthcare Improvement [IHI], 2018). In addition, “home care workers” and personal care aides are un-licensed healthcare workers who provide essential services such as companionship, assistance with activities of daily living, grocery shopping, laundry, and housekeeping to persons within the client’s home (BLS, 2019). For the purpose of this blog, home care workers and home healthcare workers are referred to as HHCWs as their service is providing care for persons within the patient’s home environment. These workers have similar occupational exposures when entering the uncontrolled home care environment.
Occupational Hazards

The National Institute for Occupational Safety and Health (NIOSH) reports occupational hazards for HHCWs include musculoskeletal disorders, latex exposure, needlesticks, bloodborne pathogen exposures, occupational stress, violence, infectious diseases, hostile pets or animals within the home or the neighborhood, temperature extremes, falls, severe weather, chemicals, pests, emotional stress, and motor vehicle travel (2010). Other researchers have echoed these hazards adding, tobacco smoke exposure, pet dander and waste, excessive dust, lifting or carrying equipment or furniture, and violence or threats from within the neighborhood (Gershon et al., 2008a, 2008b; Hittle, et al., 2016: Markkanen et al., 2014; Markkanen et al., 2017).
Researchers have shown that HHCWs have unique risks due to the uncertain and unplanned environment of a patient’s residence that are both similar and different than other healthcare environments. For instance, risks related to bloodborne pathogens is an unsurprising known hazard within the healthcare environment; however, the circumstances leading to bloodborne pathogen exposures is not the same in the home as it is in the tightly regulated and planned hospital or long-term care environment. Obstructed access, poor access due to furniture in the way, lack of working area, lack of engineered sharps safety equipment, lack of proper disposal for sharps, and unexpected interruptions from family or pets were identified as unique risks related to bloodborne pathogens in the home care environment (Hittle et al., 2016; Markkanen et al., 2014; Markkanen et al., 2017).
Participants in several studies reported musculoskeletal injuries that were precipitated by tight working spaces, awkward positions, lifting of furniture, and a lack of patient lifting equipment in the home (Agbonifo et al., 2017; Gershon et al., 2008b; Polivka et al., 2015). Working within the home environment is not the same as working within the built environment of a healthcare organization.
Mindful and Regulated Design of Healthcare Institutions
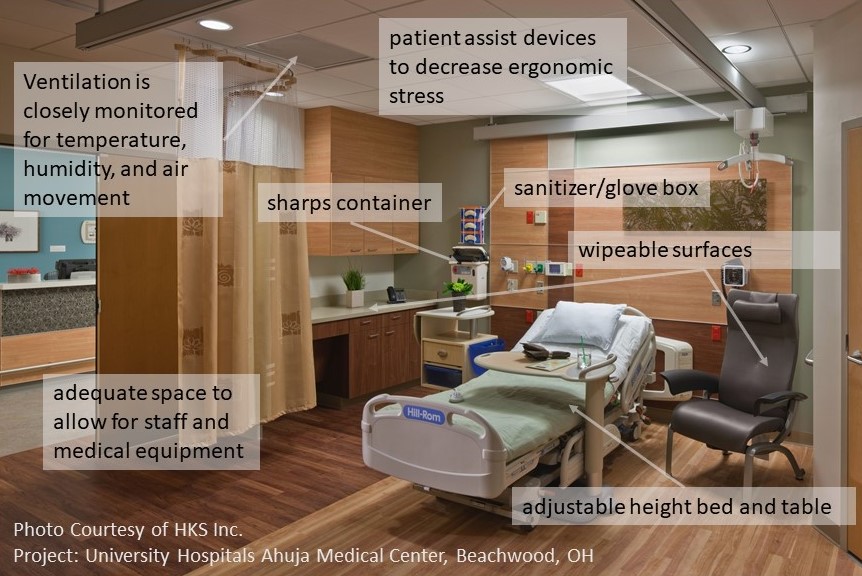
Within the acute care environment of hospitals and the long-term care environment of nursing care and rehabilitation facilities, resources from Facility Guidelines Institute (FGI) Guidelines (2018), and ANSI/ASHRAE (2017) are used by designers and regulatory bodies to support the development of safe and effective healthcare environments. The design of the built environment is focused on increasing efficiency of care, decreasing infections (e.g., wipeable surfaces, improved ventilation, mindful placement of sanitizer/glove box/sharps container) focusing on patient and staff safety and better patient outcomes. Within a healthcare organization patient room for example, there is a height adjustable bed and table, and institutions have invested in accessible patient assist devices to decrease ergonomic stress on workers. Also, there is adequate space to allow for staff and medical equipment to provide optimal patient care. Ventilation in controlled healthcare environments is closely monitored for temperature, humidity, and air movement.
The Home Healthcare Environment is Different than Healthcare Organizations
Each home is a unique work environment with hazards that could pose risks to HHCWs. For example:
Healthcare medical supplies need to be accessible for patient care. In the home environment workers have limited supplies contained in a bag they bring into the home. Often, the bag is placed on the floor or on furniture of low stature, forcing the worker to bend to access items.
There are compounding factors in the home healthcare environment. There is an array of potential compounding environmental factors in the home that are different from a controlled healthcare environment. HHCWs may encounter the presence of pets and family members. In addition, home healthcare environments may lack clean surfaces to place supplies, adequate lighting, work space, lifting equipment, specific height adjustable furniture to decrease injury to staff and patient, technology, regulation of design and planning of home healthcare environments, and support services to assist with specific duties such as housekeeping and meal prep.
Home healthcare workers enter the community and the home alone. HHCWs often work alone without immediate access to or assistance from other healthcare workers. In the home care environment, there is an absence of support departments such as safety and infection control which focus on implementation of standards, best practices, and education to protect all persons within environment.
Ventilation systems can provide comfort and decrease pathogens and respiratory irritants. Ventilation, temperature, and air quality are not monitored within the home and could pose risks to HHCWs.
Steps towards protecting Home Healthcare Workers
While there are uncertainties in home health care, there are environmental variables that can be addressed to improve worker safety. These variables include air quality, lighting, sanitation and disinfection, clear walkways and surfaces, information display for improved communication, monitoring, and the application of technology.
Improving the future of the Home Healthcare environment can engage the patient, the agency and / or the worker within two parallel strategies of adapt or modify the environment.
- Adapt to the environment, for example:
- Improve lighting by opening the blinds or bringing a task light to the patient’s home
- Decrease bending to access patient care items in the bag through the use of a raised solid wipeable surface to set the bag on
- Improve communication through the use of an app to share information
- Open a window to improve ventilation when using chemicals
- Modify the environment, for example:
- Improve lighting with different bulbs / new fixtures
- Install grab bars
- Add a portable HEPA air filter in the room
- Install an agency-provided sharps container
- Use technology to inform and monitor the patient
- Designate a specific work surface for patient care items
- Make arrangements for some furniture to be moved out of a room to create clear working space
What can the individual HHCW do to improve the work environment and decrease their occupational exposures?
- Become familiar with the hazards within the environment and the opportunities to decrease exposures. The NIOSH document Occupational Hazards in Home Healthcare provides a checklist for the HHCW and employer.
- NIOSH has created a series of 6 Fast Facts cards that provide brief explanations of individual hazards to home healthcare workers and preventative steps. These were designed to be used by employers for training and to be kept by the workers for quick reference. They are available in English, Spanish, Chinese, and Polish.
What can the employer of the HHCW do to improve the work environment?
- Complete a risk assessment of each home
- Provide recommendations on coping and adaptive strategies
- Provide resources that improve efficiency and effectiveness while improving safety
- Be part of a network of related services (social assistance, mental health, public health, etc.)
Technological advancements and changing care delivery models are expanding healthcare into the home environment. Agencies and workers that provide home care need to be cognizant of the hazards within the home and prepared with strategies to mitigate health risks to the HHCW. Assessment of each home care environment would provide insight into workplace hazards and an opportunity to plan for mitigation of occupational health risks these workers face while focusing on optimal patient outcomes. Mindfulness of the opportunities to improve the home setting without sacrificing the feel of home, will result in a safe and effective healthcare environment for the worker and the patient.
Elizabeth Bien, PhD, MSN, RN, is a Research Fellow in the Division of Biostatistics and Epidemiology, Cincinnati Children’s Hospital and Medical Center
Ron Smith, AIA, ACHA, ACHE, LEED AP, is a board-certified Healthcare Architect and Healthcare Sector Leader with LS3P Associates LTD.
This blog is part of a series hosted by NIOSH to commemorate nurses during the Year of the Nurse. The views expressed by guest authors do not necessarily reflect the views of CDC or NIOSH.
Other blogs in the series include:
- Year of the Nurse
- Managing Fatigue During Times of Crisis: Guidance for Nurses, Managers, and Other Healthcare Workers
- Nurses’ and Other Health Professionals’ Wellness and Safety Resource Update
- Surgical Smoke Inhalation: Dangerous Consequences for the Surgical Team
- Safety Culture and Health Care
- Work Ability among Older Nurses
- Can Exoskeletons Reduce Musculoskeletal Disorders in Healthcare Workers?
- Preventing Needlesticks and Sharps Injuries: Reflecting on the 20th Anniversary of the Needlestick Safety and Prevention Act
- Celebrating Nurses
References
Agbonifo, N., Hittle B., Suarez, R., & Davis, K. (2017). Occupational exposures of home healthcare workers. Home Healthcare Now, 35(3), 150-159. https://doi.org/10.1097/nhh.0000000000000509
ANSI/ASHRAE/ASHE Standard 170-2017 – Ventilation of Health Care Facilities https://www.ashrae.org/technical-resources/standards-and-guidelines/standards-addenda/ansi-ashrae-ashe-standard-170-2017-ventilation-of-health-care-facilities
FGI Guidelines 2018; Guidelines for Design and Construction of Residential Health, Care, and Support Facilities
FGI Guidelines 2018; Guidelines for Design and Construction of Guidelines for Design and Construction of Hospitals
Gershon, R. R. M., Canton, A. N., Raveis, V. H., Silver, A., Chen, C. C., Qureshi, K. A., Sherman, M., & Stone, P. W. (2008a). Household-related hazardous conditions with implications for patient safety in the home health care sector. Journal of Patient Safety, 4(4), 227-234. https://doi.org/10.1097/pts.0b013e31818936e3
Gershon, R. R. M., Porgorzelska, M., Qureshi, K. A., Stone, P. W., Canton, A. N., Samar, S. M., Westra, L. J., Damsky, M. R., & Sherman, M. (2008b). Home health care patients and safety hazards in the home: Preliminary Findings. In Henricksen, K., Battles J. B., Keyes, M. A. et al., (Eds.) Advances in Patient Safety: New Directions and Alternative Approaches. (Volume 1: Assessment). Agency for Healthcare Research and Quality.
Hittle, B., Agbonifo, N., Suarez, R., Davis, K., & Ballard, T. (2016). Complexity of occupational exposures for home health-care workers: Nurses vs. home health aides. Journal of Nursing Management, 24, 1071-1079. http://dx.doi.org/10.1111/jonm.12408
Institute for Healthcare Improvement. (2018). No place like home: Advancing the safety of Care in the home. http://www.ihi.org/resources/Pages/Publications/No-Place-Like-Home-Advancing-Safety-of-Care-in-the-Home.aspx
Markkanen, P., Quinn, M., Galligan, C., Sama, S., Brouillette, N., & Okyere, D. (2014). Characterizing the nature of home care work and occupational hazards: A developmental intervention study. American Journal of Industrial Medicine, 57(4), 445-457. https://doi.org/10.1002/ajim.22287
Markkanen, P., Galligan, C., & Quinn, M. (2017). Safety risks among home infusion nurses and other home health care providers. Journal of Infusion Nursing, 40(4), 215-223. https://doi.org/10.1097/nan.0000000000000227
National Institute for Occupational Safety and Health. (2010). Occupational health supplement: National Health Interview Survey. Figure 4: Prevalence of current asthma among U.S. adults who worked in the past 12 months. https://www.cdc.gov/niosh/topics/nhis/healthcareind/hcindfig4.html
PHI. (2019). U.S. home care workers: Key facts. https://phinational.org/wp-content/uploads/2019/08/US-Home-Care-Workers-2019-PHI.pdf
Polivka, B. J., Wills, C. E., Darragh, A., Lavender, S., Sommerich, C., & Stredney, D. (2015). Environmental health and safety hazards experienced by home health care providers: A room-by-room analysis. Workplace Health & Safety, 63(11), 512-522. https://doi.org/10.1177/2165079915610532
U.S. Bureau of Labor Statistics. (2019). Home health aides and personal care aides. Retrieved from https://www.bls.gov/ooh/healthcare/home-health-aides-and-personal-care-aides.htm#tab-2
U.S. Bureau of Labor Statistics. (2020). Employment projection. https://data.bls.gov/projections/nationalMatrix?queryParams=621600&ioType=i
Posted on by

