Safety Culture and Health Care
Posted on by Health care facilities need to foster and promote a strong culture of safety that includes a commitment to worker safety, provision of and adequate access to safety and personal protective equipment, and extensive training efforts that utilize protocols requiring specific safety actions. The American Nurses Association (2016) states that “A culture of safety describes the core values and behaviors that come about when there is collective and continuous commitment by organizational leadership, managers, and health care workers to emphasize safety over competing goals.” Similarly, the Institute for Safety and Health Management (n.d.) describes safety culture as “the attitude, beliefs, perceptions and values that employees share in relation to safety in the workplace.”
Health care facilities need to foster and promote a strong culture of safety that includes a commitment to worker safety, provision of and adequate access to safety and personal protective equipment, and extensive training efforts that utilize protocols requiring specific safety actions. The American Nurses Association (2016) states that “A culture of safety describes the core values and behaviors that come about when there is collective and continuous commitment by organizational leadership, managers, and health care workers to emphasize safety over competing goals.” Similarly, the Institute for Safety and Health Management (n.d.) describes safety culture as “the attitude, beliefs, perceptions and values that employees share in relation to safety in the workplace.”
Safety culture has several important characteristics:
- Organizations must have a commitment to provide resources to address safety concerns and to implement safe care at all times demonstrating that safety is a high priority.
- Everyone must be responsible for safety knowledge, implementation, and reporting unsafe conditions with accountability at all organizational levels.
- Organizations must recognize high-risk activities such as exposure to bloodborne and aerosol pathogens, or to chemical agents in the workplace.
- Standards for prevention of workplace injuries and good working environments must be in place and monitored.
- Input across disciplines must be sought in order to provide effective and sustained solutions to safe patient care while providing health care worker safety.
- Health care workers must believe they can report errors or near misses without fear of reprisal so that safety can be improved with continuous support and feedback rather than punishments administered.
There are five categories of work-related hazards that must be monitored, prevented and controlled in a safe and healthful work culture (Rogers, 2018) :
Biological hazards are disease producing agents (pathogens) which can be transmitted from person to person through various routes of exposure (modes of transmission) and can result in acute or chronic conditions.
Chemical hazards refer to any forms of chemicals including medications, solutions, gases, vapors, aerosols, and particulate matter that are potentially toxic or irritating to the body system.
Enviromechanical hazards are aspects of the workplace that can cause or potentiate accidents, injuries, strains, or discomfort (e.g., insufficient or inadequate equipment, hazardous flooring, poor work station design).
Physical hazards are workplace agents that can cause tissue damage by transfer of energy from the agent to the person.
Psychosocial hazards are factors in the work environment that can cause stress, strain, or interpersonal problems for the worker.
In the continuum of safety and infection prevention efforts in health care facilities, management and workers must be continuously mindful of these work-related hazards and follow a hierarchy of controls (Figure) (NIOSH, 2015) which includes hazard elimination/engineering controls, administrative and work practice controls, and use of personal protective equipment (PPE) to support a culture of safety through implementation of occupational and safety protection strategies system wide.
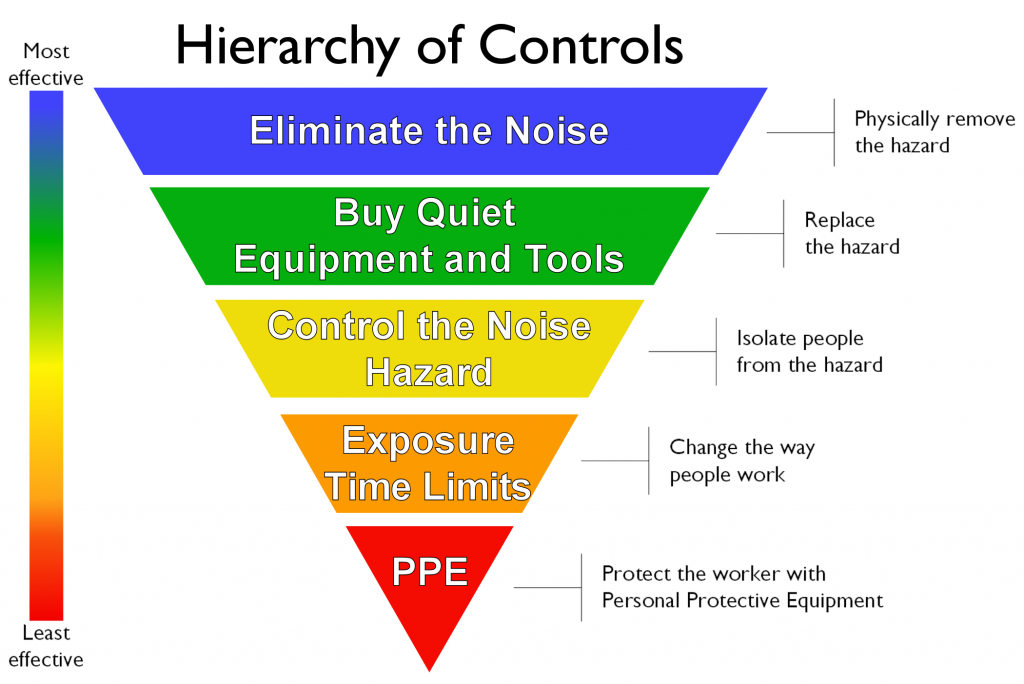
Elimination and substitution of less hazardous substances and processes and use of engineering and environmental controls such as, ventilation, negative-pressure rooms, barrier protection, and isolation rooms, are considered the first line of defense and do not rely on individual compliance. Administrative and work practice controls include the policies, standards, procedures, and practices established within an organization to limit hazardous exposures and improve worker safety. Examples include hand hygiene, cough etiquette, worker immunization policies, and training and education. While engineering and administrative strategies are the preferred prevention and control approaches for reducing health care worker infection risk, these methods are not always possible. Consequently, PPE, the last line of defense, must be employed to offer protection (Wizner, Stradtman, Novak, & Shaffer, 2016). PPE such as gloves, gowns, goggles, and respirators when needed must be provided by the organization. Every effort should be made to ensure that healthcare workers wear appropriate PPE and these “employees should feel uncomfortable when not wearing PPE during appropriate situations”(Goldfrank & Liverman, 2008, p. 8, 133); Clever, Rogers, Schultz, & Liverman, 2011).
The importance of a recognized workplace culture of safety with the goal to fully support, monitor, and sustain safe work practices and working conditions cannot be overstated. This means developing policies and procedures that effectively and proactively identify, mitigate and eliminate work-related hazards. Responsibilities are incumbent on management and health care workers to work together to achieve this continuous effort.
Bonnie Rogers, DrPH, COHN-S, FAAN, LNCC is a professor in the Department of Environmental Sciences and Engineering, North Carolina Occupational Safety and Health Education and Research Center at the UNC School of Public Health.
This blog is part of a series hosted by NIOSH to commemorate nurses during the Year of the Nurse. The views expressed by guest authors do not necessarily reflect the views of CDC or NIOSH.
Other blogs in the series include:
Managing Fatigue During Times of Crisis: Guidance for Nurses, Managers, and Other Healthcare Workers
Nurses’ and Other Health Professionals’ Wellness and Safety Resource Update
Surgical Smoke Inhalation: Dangerous Consequences for the Surgical Team
Work Ability among Older Nurses
The Unique Occupational Environment of the Home Healthcare Worker
Can Exoskeletons Reduce Musculoskeletal Disorders in Healthcare Workers?
References
American Nurses Association (2016). Culture of Safety. https://www.nursingworld.org/practice- policy/work-environment/health-safety/culture-of-safety/
Clever, L.H., Rogers, B., Schultz, A.M., & Liverman, C.T. (2011). Occupational health nurses and respiratory protection: Improving education and training. Letter Report. Washington, D.C.: The National Academies Press.
Goldfrank, L.R. & Liverman, C.T. (2008). Preparing for an influenza pandemic. Washington, D.C. : The National Academies Press.
Institute for Safety and Health Management (n.d.) Develop a Culture of Safety. http://www.ihi.org/resources/Pages/Changes/DevelopaCultureofSafety.aspx
National Institute for Occupational Safety and Health (2015). Hierarchy of controls. https://www.cdc.gov/niosh/topics/hierarchy/default.html
Rogers, B., Randolph, S.A., Mastroianni, K. (2018), 5th edition. Occupational health nursing
guidelines for primary clinical conditions. Beverly, MA.: OEM Press.
Wizner, K., Stradtman, L., Novak, D., & Shaffer, R. (2016). Prevalence of respiratory protective devices in U.S. health care facilities: implications for emergency preparedness. Workplace Health & Safety, 64(8), 359–368.
Posted on by

