Proper N95 Respirator Use for Respiratory Protection Preparedness
Posted on byWhen outbreaks of infectious disease occur, we rely on healthcare professionals to care for those affected, putting themselves at increased risk of exposure to the pathogen causing the disease. While engineering and administrative controls should be the first considerations to protect these workers from this exposure, facilities should also ensure that at-risk employees are prepared to use respiratory protection, among other personal protective equipment, should the need arise.
To aid healthcare facilities experiencing shortages of N95 respirators due to high demand across the nation, CDC developed the Strategies for Optimizing the Supply of N95 Respirators in Healthcare Settings which provides options on how to optimize supplies of disposable N95 filtering facepiece respirators (commonly called “N95 respirators”) in healthcare settings when there is limited supply. CDC prioritizes respirator use for healthcare personnel in close contact with (i.e., within 6 feet of) patients with suspected or confirmed coronavirus disease (COVID-19), during aerosol generating procedures, and for infectious diseases when airborne precautions should be followed. These activities include patient assessment for triage, entering examination rooms or patient rooms to provide care or to clean and disinfect the environment, entering a patient’s home, obtaining clinical specimens, and handling soiled medical supplies or equipment.
However, preparedness is crucial during outbreaks of disease; healthcare workers who may be called to care for COVID-19 patients, should the need arise in the future, should be fit tested if possible, medically evaluated, and training should be ongoing. To aid with these preparedness efforts, here are some reminders about proper respirator selection and use.
Filtration, Fit, and Proper Use
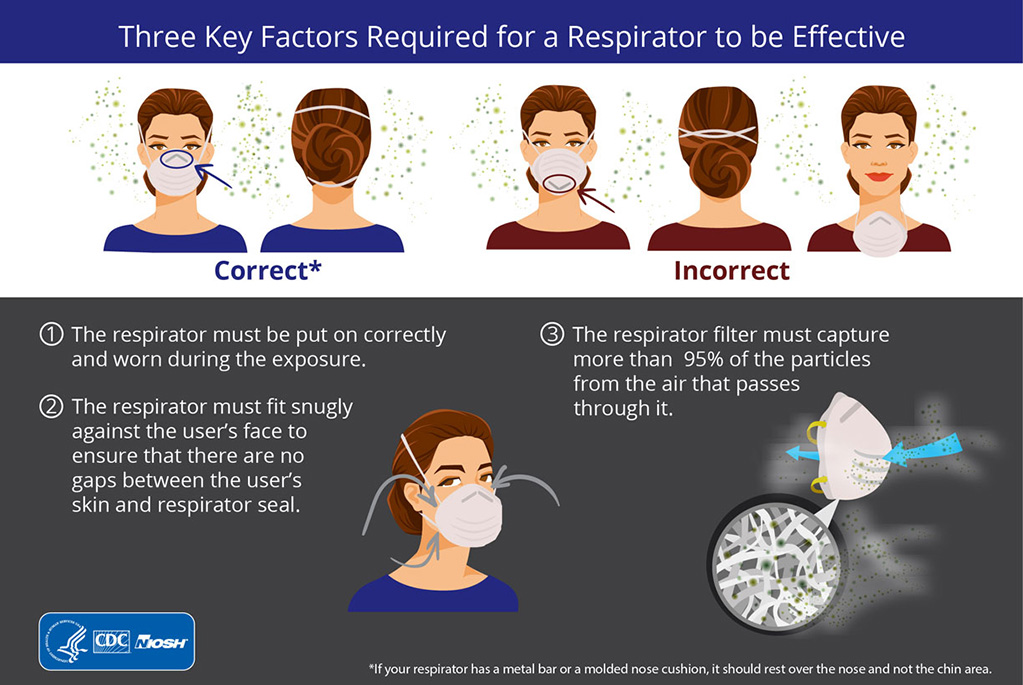
Three key criteria are required for a respirator to be effective:
1.The respirator filter needs to be highly effective at capturing particles that pass through it,
2.The respirator must fit the user’s face snugly (i.e., create a seal) to minimize the number of particles that bypass the filter through gaps between the user’s skin and the respirator seal; and
3.The respirator must be put on (donned) and taken off (doffed) correctly before and worn throughout the exposure.
(Link to infographic on the Key Factors of Respiratory Protection)
OSHA requires healthcare workers who are expected to perform patient activities with those suspected or confirmed to be infected with COVID-19 to wear respiratory protection, such as an N95 respirator. N95 respirator refers to an N95 filtering facepiece respirator (FFR) that seals to the face and uses a filter to remove at least 95% of airborne particles from the user’s breathing air. NIOSH also approves other FFRs that are as, or more, protective as the N95, including the N99, N100, P95, P100, R95, and R100. It is important to note that surgical masks, sometimes referred to as facemasks, are different than respirators and are not designed nor approved to provide protection against airborne particles. Surgical masks are designed to provide barrier protection against droplets, however they are not regulated for particulate filtration efficiency and they do not form an adequate seal to the wearer’s face to be relied upon for respiratory protection. Without an adequate seal, air and small particles leak around the edges of the respirator and into the wearer’s breathing zone.
When properly fitted and worn, minimal leakage occurs around the edges of an N95 respirator when the user inhales, ensuring that the user’s breathing air is being directed through the filter material. Staff that are required to use respiratory protection must undergo fit testing, medical clearance, and training, which are all required elements of a healthcare facility’s written respiratory protection program. These are requirements of the Occupational Safety and Health Administration (OSHA) Respiratory Protection standard (29 CFR 1910.134).
Fit testing is a critical component to a respiratory protection program whenever workers use tight-fitting respirators. OSHA requires an initial respirator fit test to identify the right model, style, and size respirator for each worker. Annual fit tests ensure that users continue to receive the expected level of protection. A fit test confirms that a respirator correctly fits the user. Additionally, tight-fitting respirators, including N95s, require a user seal check each time you put one on to help ensure the best fit possible. In the US, NIOSH-approved respirators include instructions on how to conduct a user seal check.
During times of extreme supply constraints, when there may be limited availability of respirators or fit test kits, employers may face challenges in fit testing workers. Employers should make every effort to ensure that workers who need to use tight-fitting respirators are fit tested to identify the right respirator for each worker.
Fit Under Fire: Situational Strategies to Achieve the Best Respirator Fit During Crisis
Under serious outbreak conditions in which respirator supplies are severely limited, however, you may not have the opportunity to be fit tested on a respirator before you need to use it. While this is not ideal, in this scenario, you should work with your employer to choose the respirator that fits you best, as, even without fit testing, a respirator will provide better protection than a facemask or using no respirator at all. If possible, start with the size you have been fit tested for previously, but as size can vary by manufacturer and model, you may need to wear a different size to achieve a good fit. (If you have never been fit tested before, the following recommendations are still useful.) The respirator should fit over your nose and under your chin. If you cannot get a good face seal, try a different model or size. If you receive respirators, and you need to use them right away without fit testing, ask your employer for additional (you should have already received training on proper respirator use and user seal checks) product training videos and literature on proper donning and doffing, which should be available from the manufacturer. Practice putting on the respirator and doing a user seal check at least several times. Check the fit in a mirror or ask a colleague to look to be sure the respirator is touching your face and appears to be on properly. While fit testing is ideal to confirm if a respirator does or does not fit, healthcare professionals should be able to obtain a good fit if they have had training and they perform a user seal check prior to each use of the respirator.
Even if workers begin using respirators without proper fit testing, employers should make every effort to perform fit testing as respirator supplies allow. Employers should always perform fit testing for workers who cannot successfully seal check their own respirators.
In addition to a user seal check, properly donning the respirator in the first place will help to achieve a good fit. Here are some additional considerations when donning your respirator:




- Place the respirator over your nose and under your chin. If the respirator has two straps, place one strap below the ears and one strap above. If you’re wearing a hat, it should go over the straps.
- If the respirator has a noseclip (a thin metal bar at the top of the device), use your fingertips from both hands to mold the noseclip firmly against your nose and face. Do not pinch with one hand.
- Be sure to conduct a user seal check every time you put on the respirator. This should be done before you enter a patient room. Your respirator may have instructions on how to conduct a user seal check.
- Facial hair will cause the respirator to leak, so users should be clean-shaven. Some types of facial hair are acceptable as long as the facial hair does not lie along the sealing area of the respirator.
- If you feel dizzy, lightheaded, or nauseated, leave the patient room, remove your respirator, and get medical attention.
- Discard the respirator when: (1) it becomes more difficult to breathe through it, (2) if it becomes dirty or (3) the respirator becomes damaged.
- Do NOT TOUCH the front of the respirator! It may be contaminated.
- Keep your respirator clean and dry. Be sure to read and follow the manufacturer’s recommendations on use and storage.
- If supplies are short, facilities should consider applying the appropriate strategies identified in the CDC Strategies for Optimizing the Supply of N95 Respirators.
You can find additional information on how to protect healthcare workers in times of outbreak by regularly visiting the CDC’s Coronavirus information for Healthcare Professionals webpage.
Maryann M. D’Alessandro, PhD, is the Director of the NIOSH National Personal Protective Technology Laboratory
Jaclyn Krah Cichowicz, MA, is a Health Communications Specialist in the in the NIOSH National Personal Protective Technology Laboratory.
Other Resources
Proper Use, Filtration, and Fit – The Three-Legged Stool of Respiratory Protection (Blog)
Required Labeling of a NIOSH-Approved N95 Filtering Facepiece Respirator Infographic
Key Factors of Respiratory Protection Infographic
NIOSH Respirator Filter Classes Infographic
A Particle is a Particle (Video)
N95 Respirators and Surgical Masks (Blog)
Understanding the Difference: Surgical Masks and N95 Respirators Infographic
How to Properly Put on or Take off a Disposable Respirator (Instruction sheet)
Hospital Respiratory Protection Program Toolkit
Filtering out Confusion: Fit Testing (Fact Sheet)
Filtering out Confusion: User Seal Check (Fact Sheet)
Donning, Doffing, and User Seal Checks (Video)
To Beard or not to Beard, That’s a Good Question (Blog)
CDC’s Strategies for Optimizing the Supply of N95 Respirators
The Centers for Disease Control and Prevention is addressing questions related to the Coronavirus Disease 2019 through CDC-INFO and on their webpage. As such, this blog has been closed to comments. Please visit https://www.cdc.gov/coronavirus/2019-ncov/index.html. You can find the most up-to-date information on the outbreak and get the latest answers to frequently asked questions. If you have specific inquiries, please contact CDC-INFO at https://wwwn.cdc.gov/dcs/contactus/form or by calling 800-232-4636. If you have questions about PPE that are not related to Coronavirus Disease 2019, please contact us at PPEConcerns@cdc.gov.
Posted on by

