Lighting Interventions to Reduce Circadian Disruption in Rotating Shift Workers
Posted on by
Shift work has been linked to poor sleep, chronic metabolic disorders (e.g., cardiovascular disease, diabetes, and obesity), several forms of cancer [1-3], depression, and elevated risk for the occurrence of accidents. These risks are especially acute for those who work rotating shifts that involve working through the night [4-8], as sometimes occur in hospitals. Studies show that healthcare workers are at greater risk for shift-work-related health and safety problems compared to their colleagues who work conventional daytime hours [9-11]. To make matters more complex, nurses typically follow 12-hour shift schedules and can perform crucial tasks (e.g., monitoring unstable patients, etc.) when alertness levels are low and the pressure for sleep is high. Researchers from Mt. Sinai and Rensselaer Polytechnic Institute examined the effects of an experimental lighting intervention on levels of melatonin, task performance, activity–rest patterns, and subjective sleep quality.
Background
Research conducted over the last 40 years has found a strong link between health problems and disruption of the human circadian system [12, 13], which regulates our bodily processes like sleeping by producing circadian rhythms that basically signal the body to do the right things at the right times. Because the human circadian system runs on a cycle that, for most people, is slightly longer than the solar day, it must be continually synchronized to keep the right things happening at the right times.
The circadian system’s main synchronizer is the 24-hour pattern of light and dark reaching our eye retina, which sends those signals via the optic nerve to a cluster of cells in the brain’s hypothalamus region called the master biological clock, which in turn regulates circadian rhythms. Although several properties of light are known to influence the timing of the circadian system [14, 15], a key property for our study is a light source’s spectral composition, or its wavelength. Short-wavelength light is the most-effective of all light sources for stimulating the circadian system, perhaps best visualized as the blue light of the morning sky that energizes us for the coming day. Long-wavelength light, on the other hand, has negligible effects on the circadian system and is perhaps best visualized as the red sky at twilight that is followed by sleep.
The Study
In this study, we evaluated the effectiveness of experimental lighting interventions in terms their effects on the participants’ levels of the hormone melatonin, which is produced in darkness and prepares the body for sleep. Blue light suppresses melatonin production at night, while red light does not. But when experienced at sufficiently high levels at any time of day, both types of light can elicit a beneficial, immediate alerting effect that is similar to drinking a cup of coffee. We also assessed the lighting’s effect on task performance, activity–rest patterns, and subjective sleep quality.
Our study took place in four hospitals in Albany, NY, Schenectady, NY, South Bend, IN, and Syracuse, NY. One of the interventions explored a novel lighting intervention (red light), delivered to the participants’ retinas via personal light glasses, that was designed to increase alertness and improve performance without disrupting the secretion of melatonin. Based on our previous research [16-19], we hypothesized that the red light would be useful for promoting workplace alertness without negatively affecting the sleep and the circadian system. Seventy-eight participants (49 on day shift, 29 on night shift) completed at least 4 weeks (2 weeks baseline and 2 weeks intervention) of the study’s 20-week protocol.
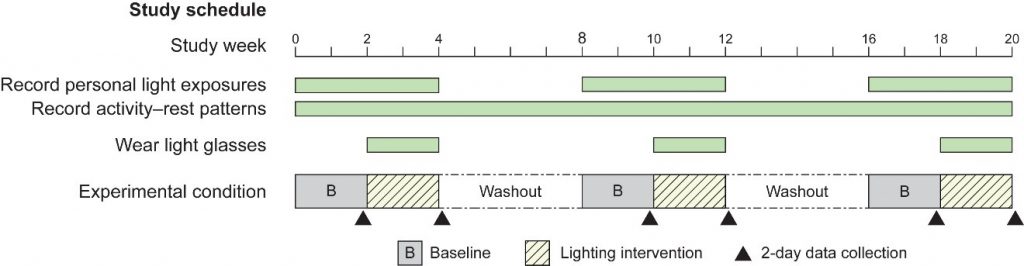
After the baseline data collection, participants were exposed to either 30 minutes of circadian-ineffective red light, circadian-effective blue light, or dim white light (the experimental control) during the beginning, middle, and end of their shifts for 2 consecutive weeks. On the last 2 shifts of the intervention period, the participants underwent computer-based auditory performance tests, submitted saliva samples for melatonin and cortisol assay prior to and immediately after the light exposures, and completed questionnaires relating to feelings of sleepiness during the testing, as well as sleep quality and sleep disturbance over the past week. Activity–rest patterns and personal light exposures were also continuously monitored via experimental devices routinely employed in our research (Figure 1).
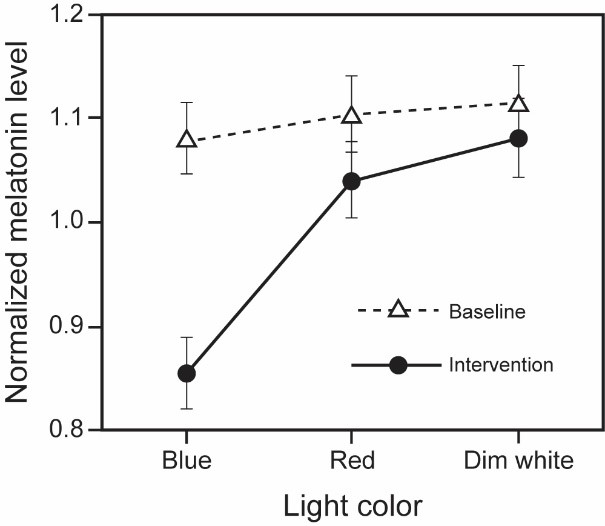
The study’s results were mostly positive and consistent with our hypotheses. Only the blue light suppressed participants’ nighttime melatonin levels (Figure 2), as expected, but the performance testing results were mixed. While some positive effects of red light were shown at the end of the day shift and in the middle of the night shift, when workers are likely to be most tired, not all of the performance results were in the expected direction and there were large amounts of missing data. This is understandable, given the challenges of gathering data from busy nurses while they were working. Sleep outcomes improved for night shift-nurses exposed to the red and blue light compared to the dim control. Notably, the nurses who were exposed to the blue light experienced better quality sleep, which is consistent with our hypothesis that blue light promotes synchronization between our circadian rhythms and the solar day’s 24-hour pattern of light and dark.
This is the first field study to show that red light can be used to improve sleep and improve certain types of performance in real-life work situations without affecting nighttime melatonin levels. Future studies should focus on implementing the study’s red-light intervention as less-intrusive, ambient workplace lighting to better ensure participant compliance. For additional resources related to this research, see this presentation and this website.
We would like to hear from you if you have comments or questions about our research. Please give your feedback in the comment section below.
Mariana G. Figueiro, PhD, Department of Population Health Science and Policy, Icahn School of Medicine at Mount Sinai
David Pedler, Lighting Research Center at Rensselaer Polytechnic Institute
This study was funded by grant R01OH01668 from the National Institute for Occupational Safety and Health (NIOSH). This blog is part of a series highlighting extramural research funded by NIOSH through the Office of Extramural Programs.
References
- Schernhammer ES, Laden F, Speizer FE, Willett WC, Hunter DJ, Kawachi I. Night-shift work and risk of colorectal cancer in the Nurses’ Health Study. J Natl Cancer Inst. 2003;95:825-88. doi: 10.1093/jnci/95.11.825
- Papantoniou K, Devore EE, Massa J, Strohmaier S, Vetter C, Yang L, et al. Rotating night shift work and colorectal cancer risk in the nurses’ health studies. Int J Cancer. 2018;143(11):2709-17. doi: 10.1002/ijc.31655
- Åkerstedt T, Knutsson A, Narusyte J, Svedberg P, Kecklund G, Alexanderson K. Night work and breast cancer in women: a Swedish cohort study. BMJ open. 2015;5(4):e008127. doi: 10.1136/bmjopen-2015-008127
- Kecklund G, Axelsson J. Health consequences of shift work and insufficient sleep. BMJ. 2016;355:i5210. doi: 10.1136/bmj.i5210
- Caruso CC. Negative impacts of shiftwork and long work hours. Rehabil Nurs. 2014;39(1):16-25. doi: 10.1002/rnj.107
- Knutsson A, Kempe A. Shift work and diabetes – a systematic review. Chronobiol Int. 2014;31(10):1146-51. doi: 0.3109/07420528.2014.957308
- Wagstaff AS, Sigstad Lie JA. Shift and night work and long working hours–a systematic review of safety implications. Scand J Work Environ Health. 2011;37(3):173-85. doi: 10.5271/sjweh.3146
- Wang X, Armstrong M, Cairns B, Key T, Travis R. Shift work and chronic disease: the epidemiological evidence. Occup Med. 2011;61(2):78-89. doi: 10.1093/occmed/kqr001
- Schernhammer ES, Laden F, Speizer FE, Willett WC, Hunter DJ, Kawachi I, et al. Rotating night shifts and risk of breast cancer in women participating in the Nurses’ Health Study. J Natl Cancer Inst. 2001;93(20):1563-8. doi: 10.1093/jnci/93.20.1563
- Gu F, Han J, Laden F, Pan A, Caporaso NE, Stampfer MJ, et al. Total and cause-specific mortality of U.S. nurses working rotating night shifts. Am J Prev Med. 2015;48(3):241-52. doi: 10.1016/j.amepre.2014.10.018
- Ferri P, Guadi M, Marcheselli L, Balduzzi S, Magnani D, Di Lorenzo R. The impact of shift work on the psychological and physical health of nurses in a general hospital: A comparison between rotating night shifts and day shifts. Risk Manag Healthc Policy. 2016;9:203-11. doi: 10.2147/RMHP.S115326
- Smolensky MH, Hermida RC, Reinberg A, Sackett-Lundeen L, Portaluppi F. Circadian disruption: New clinical perspective of disease pathology and basis for chronotherapeutic intervention. Chronobiol Int. 2016;33(8):1101-19. doi: 10.1080/07420528.2016.1184678
- Zimmet P, Alberti KGMM, Stern N, Bilu C, El-Osta A, Einat H, et al. The Circadian Syndrome: is the Metabolic Syndrome and much more! J Intern Med [Internet]. 2019. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/joim.12924.
- Rea MS, Figueiro MG, Bullough JD, Bierman A. A model of phototransduction by the human circadian system. Brain Res Rev. 2005;50(2):213-28. doi: 10.1016/j.brainresrev.2005.07.002
- Duffy JF, Czeisler CA. Effect of light on human circadian physiology. Sleep Med Clin. 2009;4(2):165-77. doi: 10.1016/j.jsmc.2009.01.004
- Figueiro MG, Bierman A, Plitnick B, Rea MS. Preliminary evidence that both blue and red light can induce alertness at night. BMC Neurosci. 2009;10:105. doi: 10.1186/1471-2202-10-105
- Plitnick B, Figueiro MG, Wood B, Rea MS. The effects of red and blue light on alertness and mood at night. Lighting Res Technol. 2010;42(4):449-58. doi: 10.1177/1477153509360887
- Figueiro MG, Rea MS. The effects of red and blue lights on circadian variations in cortisol, alpha amylase, and melatonin. Int J Endocrinol. 2010;2010:829351. doi: 10.1155/2010/829351
- Figueiro MG, Sahin L, Roohan C, Kalsher M, Plitnick B, Rea MS. Effects of red light on sleep inertia. Nat Sci Sleep. 2019;11:45-57. doi: 10.2147/NSS.S195563
Posted on by

