Geography, Genetics and Leading Causes of Death
Posted on by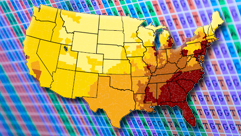 In the United States, the 5 leading causes of death are heart disease, cancer, chronic lower respiratory diseases, cerebrovascular diseases (stroke), and unintentional injuries. On May 2, 2014, the Centers for Disease Control and Prevention released an MMWR report on the annual number of potentially preventable deaths from these 5 causes in the United States. The data suggest that at least a third of those deaths every year are potentially preventable. The analysis compared the number of observed deaths in each state with an expected number that is based on average death rates for the three states with the lowest rates for each cause. States in the Southeast had the highest number of potentially preventable deaths. Therefore, potentially a large health impact may be achieved if states with higher rates were able to reduce the prevalence of risk factors for leading causes of death to the average of the three lowest states. Nevertheless, press coverage of this important report tended to sensationalize and overinterpret the results of these types of analyses with statements like “Living in the Southeast is bad for your health”; or “lifespan to do more with geography than genetics”.
In the United States, the 5 leading causes of death are heart disease, cancer, chronic lower respiratory diseases, cerebrovascular diseases (stroke), and unintentional injuries. On May 2, 2014, the Centers for Disease Control and Prevention released an MMWR report on the annual number of potentially preventable deaths from these 5 causes in the United States. The data suggest that at least a third of those deaths every year are potentially preventable. The analysis compared the number of observed deaths in each state with an expected number that is based on average death rates for the three states with the lowest rates for each cause. States in the Southeast had the highest number of potentially preventable deaths. Therefore, potentially a large health impact may be achieved if states with higher rates were able to reduce the prevalence of risk factors for leading causes of death to the average of the three lowest states. Nevertheless, press coverage of this important report tended to sensationalize and overinterpret the results of these types of analyses with statements like “Living in the Southeast is bad for your health”; or “lifespan to do more with geography than genetics”.
The CDC report acknowledges that “death rates are population health outcome measures that reflect the combined influences of multiple biological and social health determinants, public health efforts, and medical care” In fact, both zip codes and genetic codes are important for our health. Genetic factors are known to play a role in nine of the Ten Leading Causes of Death in the United States, most notably chronic diseases such as cancer and heart disease. Most human disease results from the interaction of our genetic susceptibility with environmental and behavioral risk factors, such as diet, physical activity, infectious agents and the physical environment. Advances in genomics in the past two decades are increasingly allowing us to learn more about the relationship between genes, environment, and behaviors, and why some people get sick under certain conditions, while others do not. A family health history provides information that can help to identify people who may have a higher risk for certain diseases and for who need targeted medical or lifestyle interventions are needed.
While promises of genomic technologies to improve health may have been hyped and oversold in the past, we are now seeing the leading edge for applications of whole genome sequencing in health practice both for the detection and control of infectious disease outbreaks and for the diagnosis of people with rare diseases. Although much of the field will be a work in progress for quite some time, an increasing number of applications can actually be used now to improve health and prevent disease in the US and worldwide. The CDC Office of Public Health Genomics developed an evidence-based classification schema for human genomic applications in medical and population settings. The schema takes a population perspective for an emerging role for public health programs to supplement clinical practice. One may be surprised to see on this list several applications that are supported by recommendations from evidence panels. In addition to newborn screening, which is the largest public health genetics program in the world, an increasing number of recommended applications are being regularly added to the list. For example, there are currently about 2 million persons in the US affected with one of three genetic conditions that put them at increased risk for early heart attacks and cancer. Most affected individuals are not aware of their risk and there are evidence-based interventions that can significantly reduce their risk. A combined public health and healthcare approach could provide access to genetic evaluation and preventive interventions in relatives of affected patients. These applications are only the tip of the iceberg for what’s to come in the next decade. New fields like epigenetics are blurring the boundaries between genetic and environmental factors. Also, we are finding not only how our genes influence our response to the environment but also how our environment affects gene expression and transmission throughout life and across generations. New approaches such as metagenomics and the study of the microbiome are allowing us to explore the contribution of multitude of genomes to health and disease.
In conclusion, genomics will increasingly provide targeted or stratified approaches to improving health and preventing disease that can inform and supplement population strategies such as policy changes. Ideally, improving health should rely on complementary efforts using all forms of evidence based interventions to reduce the burden of disease and premature death.
Posted on by


