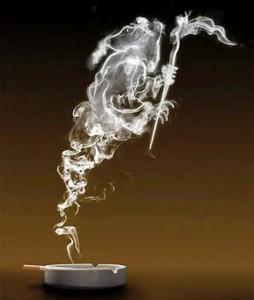
Smoke Screen…
Posted on by
Never Let Genetics Blind You to the Harsh Reality of Cigarettes
The emerging field of genomics might one day provide some tools to help address the smoking epidemic. However, smokers should never think that their genes can protect them from devastating harms or provide an easy way for them to quit later.
In 2012, CDC started a national media campaign to encourage smokers to quit and prevent others, especially young people, from starting. The new communications initiative is different from past efforts because it includes graphic depictions of the real life damage that smoking does. This campaign continues in 2013 with tips from former smokers. “Although they may be tough to watch, the ads show real people living with real, painful consequences from smoking,” said CDC Director Thomas R. Frieden. ” There is sound evidence that supports the use of these types of hard-hitting images and messages to encourage smokers to quit, to keep children from ever beginning to smoke, and to drastically reduce the harm caused by tobacco.”
Where There is Smoke There is Fire… Addiction, and Yet Desire To Quit
 Last fall, CDC’s MMWR provided the latest data on cigarette smoking among working U.S. adults. Smoking remains the single most important preventable cause of disease and death in the U.S., yet people of all descriptions, occupations, and backgrounds are addicted to nicotine. Most want to stop, but find it very difficult. More than one half had made an attempt to quit in the past year.
Last fall, CDC’s MMWR provided the latest data on cigarette smoking among working U.S. adults. Smoking remains the single most important preventable cause of disease and death in the U.S., yet people of all descriptions, occupations, and backgrounds are addicted to nicotine. Most want to stop, but find it very difficult. More than one half had made an attempt to quit in the past year.
In recent years, more attention has been paid to the potential contribution of one’s genes to the risks of smoking addiction and harms. To rephrase a common saying among geneticists: “Genes spill the fuel, but environment lights the match.” In other words, one’s genome may predispose one to risk for certain diseases, but it is only when that vulnerability is combined with certain exposures that harm occurs. Among behaviors that impact the incidence of disease, smoking is one of the most powerful “fire starters” in the world. Some have argued that awareness of increased genetic risk (e.g., through family health history or valid genetic test) could lead some people to make positive changes in their behaviors including smoking cessation. The good news is that people who do stop smoking sharply reduce their risk for disease and early death, and the earlier they stop, the better.
Where There is Smoke There is High Risk
“But my great aunt smoked every day and lived to be 100!”
The existence of centenarian smokers simply reflects the fact that, among a population of millions, even the longest odds can permit the survival of a few. There are also unwise, unbelted, but fortunate car passengers who somehow live through horrific accidents despite having greatly reduced their chances {always buckle up!}. There are even documented cases of people who have fallen from skyscrapers and even high altitude aircraft and survived, but we don’t recommend that either.
Regardless of age, however, smoking takes a toll on quality of health and harms virtually every organ in the body, not to mention the effects on family members and others of secondhand smoke. For children aged 18 months or younger, secondhand smoke exposure is responsible for an estimated 150,000–300,000 new cases of bronchitis and pneumonia and approximately 7,500–15,000 hospitalizations, annually in the United States alone.
No Easy Answers Through Genetics
 Tobacco smoke is a mixture of more than 7,000 chemicals that interact with the body through multiple complex pathways. Hundreds of these chemicals are toxic or carcinogenic. Genetic research on smoking and health has focused on three main areas: 1) understanding molecular mechanisms of smoking-related diseases, including lung cancer; 2) using combinations of risk factors, including genetic susceptibility, to identify high-risk groups of smokers for enrollment in chemoprevention and screening trials; and 3) tailoring smoking cessation programs to individuals based on genetic risk information. Although all remain active areas of research, none have so far changed the public health or clinical approaches to preventing smoking-related diseases. In fact, an article recently published in Annals of Family Medicine notes that all proven interventions for treating tobacco dependence—such as quit lines and physician counseling—are underutilized. The authors conclude that “although genetics offers increasing opportunities to tailor drug treatment, and may in some cases provide useful risk prediction, other methods of personalizing care are likely to yield greater benefit to populations experiencing health disparities related to tobacco use.”
Tobacco smoke is a mixture of more than 7,000 chemicals that interact with the body through multiple complex pathways. Hundreds of these chemicals are toxic or carcinogenic. Genetic research on smoking and health has focused on three main areas: 1) understanding molecular mechanisms of smoking-related diseases, including lung cancer; 2) using combinations of risk factors, including genetic susceptibility, to identify high-risk groups of smokers for enrollment in chemoprevention and screening trials; and 3) tailoring smoking cessation programs to individuals based on genetic risk information. Although all remain active areas of research, none have so far changed the public health or clinical approaches to preventing smoking-related diseases. In fact, an article recently published in Annals of Family Medicine notes that all proven interventions for treating tobacco dependence—such as quit lines and physician counseling—are underutilized. The authors conclude that “although genetics offers increasing opportunities to tailor drug treatment, and may in some cases provide useful risk prediction, other methods of personalizing care are likely to yield greater benefit to populations experiencing health disparities related to tobacco use.”
There are NO validated genetic tests that can tell someone that they have a lower risk of health effects from smoking. Smoking is fundamentally harmful to health regardless of genetic makeup or family history. No amount of exposure to tobacco smoke is without risk, and no genetic test provides an excuse to smoke.
Research investigating the contribution of genetics to smoking addiction and harms continues to progress, but there are no known genes which make smoking less harmful or easier to quit. Smokers who believe that their genes can protect them are gambling with their lives against tremendous odds.
Posted on by



