A New Vision for Using Genomics to Improve Health: An Expanded Role for Public Health
Posted on by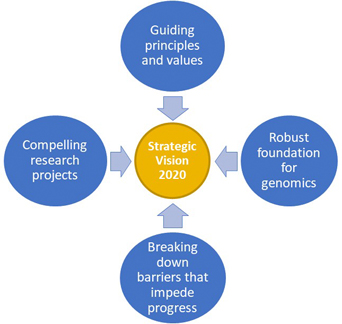 The National Human Genome Research Institute (NHGRI) recently published a new strategic vision 2020 to identify research priorities and opportunities in human genomics for improving health. The framework includes four main areas: guiding principles and values, a robust foundation for genomics, breaking down barriers that impede progress, and compelling research projects.
The National Human Genome Research Institute (NHGRI) recently published a new strategic vision 2020 to identify research priorities and opportunities in human genomics for improving health. The framework includes four main areas: guiding principles and values, a robust foundation for genomics, breaking down barriers that impede progress, and compelling research projects.
Since the completion of the human genome project, genomics has played an increasingly important role in biomedical and public health research. This has led to new genomic tests and applications, such as tumor genome analysis for targeted therapeutics, non-invasive prenatal testing, and genomic tests for childhood conditions and rare disorders.
After the last NHGRI strategic planning cycle, in 2011, the Centers for Disease Control and Prevention developed a public health vision and priority actions to use human genomics to save lives. The 2020 NHGRI vision moves the needle significantly beyond that of 2011 in terms of applications of human genomics in improving the health of individuals and populations. In the accompanying table, we summarize elements of the 2020 strategic plan for which key public health approaches will be needed to fulfill the promise of human genomics to improve health for all.
An Expanding Role for Public Health Sciences
A population perspective is needed to assess how genomics fits in an overall ecological model of health and disease that considers not only our genes but also environmental, behavioral, and social determinants of health. Since common chronic diseases with global health impact have known environmental, social, and behavioral determinants (e.g., tobacco use; physical activity; diet; racial, ethnic, and economic factors; and differential access to health care), it is important to assess the benefits, harms and costs of genome-based interventions in prevention and control of these diseases. Applying genomic tools in practice will require a multidisciplinary research collaboration with public health scientists (e.g., epidemiologists; behavioral, social, and communication scientists; health services researchers).
A barrier to using genomics to improve health and preventing disease is the lack of optimal uptake of evidence-based interventions. CDC has developed and maintains a database of all genomics guidelines and recommendations by level of evidence, based on the availability of evidence-based recommendations and systematic reviews. As of November 3, 2020, there are 98 tier 1 genomic applications (those with evidence-based recommendations based on systematic reviews). Implementation science approaches are needed to identify the most effective methods and strategies for facilitating the use of genomic applications in practice. Partnerships between health care organizations and public health programs can bridge the implementation gap and reduce health disparities. Recent public health activities highlight the science impact of public health programs in accelerating the identification of individuals with hereditary cancers in populations, and in developing implementation science metrics for public health programs.
An Expanding Role for Public Health Programs
To date, Newborn screening for treatable inherited conditions represents the most successful approach for public health, but population screening across the lifespan for other genetic conditions is increasingly possible. Selected tier 1 genomic applications (Lynch syndrome, hereditary breast and ovarian cancer, and familial hypercholesterolemia) can identify people at risk in health systems and through testing relatives of affected individuals (cascade screening). State public health programs will have a strong leadership role in providing effective communication to providers and the general public about evidence-based recommendations (e.g. state cancer public health programs). Public health programs will also help monitor implementation of genomic medicine, quantify health disparities in implementation and develop approaches to address them.
Other emerging applications include genetic predisposition to adverse drug effects (pharmacogenomics), carrier testing of prospective parents, and use of polygenic risk scores in disease detection and prevention. In addition, as millions of people have sought direct-to-consumer genetic tests, public health programs can help educate the general public about the promise and limitations of emerging tests in improving health, as well as to track the impact of genomic tests at the population level.
Will Human Genomics Be Finally Integrated into Routine Healthcare?
At the end of the 2020 strategic vision document, NHGRI offers 10 bold predictions for 2030. Recommendation number 6 echoes a similar prediction made in 1999 for the practice of medicine in 2010.
“The regular use of genomic information will have transitioned from boutique to mainstream in all clinical settings, making genomic testing as routine as complete blood counts.”
Obviously, the field of genomics moved rapidly in the past decade, even though the ultimate promise of genomics in improving human health is still work in progress. The bold prediction for 2030 will require a comprehensive approach that includes public health sciences and programs to maximize the value of genomics in improving health for all.
We invite our readers to submit input and feedback on how public health can contribute to the success of genomics for the years to come.
Please submit your comments below…
Selected Areas for Public Health Partnership from the New NHGRI 2020 Strategic Plan at the Forefront of Genomics.
| Guiding principles and values for human genomics |
|---|
|
| Sustaining and improving a robust foundation for genomics |
|
| Breaking down barriers that impede progress in genomics |
|
| Compelling genomics research projects in biomedicine |
|
Posted on by


