Dear John, There’s no point in waiting any longer. Let’s call it quits…
Posted on by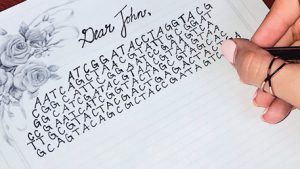 In 1999, Dr. Francis Collins, director of the Human Genome Project, provided a bold vision for what the practice of genomic medicine might soon look like. Collins described the case of a hypothetical man named “John,” a 23 year-old smoker living a decade into the future in 2010. “His substantial risk of contracting lung cancer provides the key motivation for him to join a support group of persons
In 1999, Dr. Francis Collins, director of the Human Genome Project, provided a bold vision for what the practice of genomic medicine might soon look like. Collins described the case of a hypothetical man named “John,” a 23 year-old smoker living a decade into the future in 2010. “His substantial risk of contracting lung cancer provides the key motivation for him to join a support group of persons
…genomics would, in the not too distant future, move beyond basic research and become a real tool to save millions of lives.
at genetically high risk for serious complications of smoking, and he successfully kicks the habit.” Through the example of smoking, the point was made that genomics would, in the not too distant future, move beyond basic research and become a real tool to save millions of lives. Worldwide, tobacco use, was (and is) the leading cause of preventable death. In the U.S. alone, 46.5 million (23.5%) adults were smokers in 1999. Despite the problem’s magnitude, however, many scientists and public health practitioners were skeptical that an investment in genomics could ever pay off.
In 2012, two years after John’s story was to play out, we reviewed the state of the science for genomics and smoking cessation in our blog, Smoke Screen. We reported that, despite progress, there were still no validated genetic tests ready to address the problem of smoking, and that no one should use a genetic test result or family history as a reason not to quit. However, there had been some progress in genomics research in three main areas: understanding molecular mechanisms of smoking-related diseases, using genetic susceptibility to begin to identify higher risk groups of smokers, and tailoring smoking-cessation programs to individuals. Meanwhile, many Americans needed no genetic test to stop smoking. In 2012, the number of smokers had declined to 42.1 million (18.1%) U.S. adults.
 So where are we in 2018?
So where are we in 2018?
In January of this year, CDC released the latest data revealing that in 2016 almost 38 million (15.5%) U.S. adults were current cigarette smokers. The new numbers demonstrated further public health success – but also that room for substantial improvement remains. Meanwhile, research continues into how to reduce tobacco use and risk. With our regularly updated and searchable Public Health Genomics Knowledge Base (PHGKB), we try to stay on top of the developments in the field of genomics and smoking cessation. While we still don’t have a scientific breakthrough, several recent articles regarding genomics and smoking are noteworthy.
- Pharmacogenomic nicotine replacement therapy. One small study assessed factors influencing the impact of pharmacogenomic prescribing on adherence to nicotine replacement therapy (NRT). Pharmacogenomics is the study of genetic variation as a factor in drug response, affecting both safety and effectiveness. The qualitative study of 40 participants aimed to explore the impact of pharmacogenomic prescribing of NRT on smoker’s expectations of quitting successfully and perceived differences from previous attempts. The researchers concluded that, in the small study group, pharmacogenomic NRT prescribing was not especially remarkable to participants and did not seem to influence their adherence to NRT.
- Genomic applications. Another article reviewed genomic applications considered for implementation, including the CHRNA5 genetic test for disease risk, smoking cessation treatment, and for motivating smoking behavior change. For these genomic applications, the authors regarded evidence for analytic validity and clinical validity favorably but viewed evidence for clinical utility as inadequate and called for more work in that area.
- Relevance of the CHRNA5 and CYP2A6 genes. Another article reviewed the relevance of the CHRNA5 and CYP2A6 genes as important to risk of smoking heaviness, tobacco use disorder, and smoking-related diseases in humans. The authors also described the evidence of analytical and clinical validity for the applications and state that evidence around clinical utility is growing. The authors argue that the biomarkers have the potential of determining elevated disease risk in smokers, personalizing cessation treatments, and for motivating behavioral changes. The authors also make the case that healthcare should prepare for the predicted integration of anticipated genomic applications for patients who smoke .

New genomics research provides hope for smoking cessation, but we’re not there yet.
Promising, new genomics research provides hope that Dr. Collins’ precision medicine vision will one day be realized for smoking cessation. Until that time, however, our conclusion remains the same. There are still NO validated genetic tests that can help smokers kick the habit. Smoking is fundamentally harmful to health regardless of one’s genetic makeup or family history.
Dear John, Don’t miss the opportunity for better health and a better life!
So here’s our advice for “John” (and for all real-life smokers):
Dear John,
You’re 31 now. Every year that goes by, and you remain a smoker, is a year of missed opportunity for better health and a better life. About a half a million Americans die every year from smoking. However, if you quit now, you can substantially lower your health risks and add years to your life! Please don’t wait for a genetic test to be ready before seeking help to quit. Your life is too valuable.
Thank you.
As always, we welcome your comments.
Posted on by


