Precision Health Innovations in the Pandemic Era
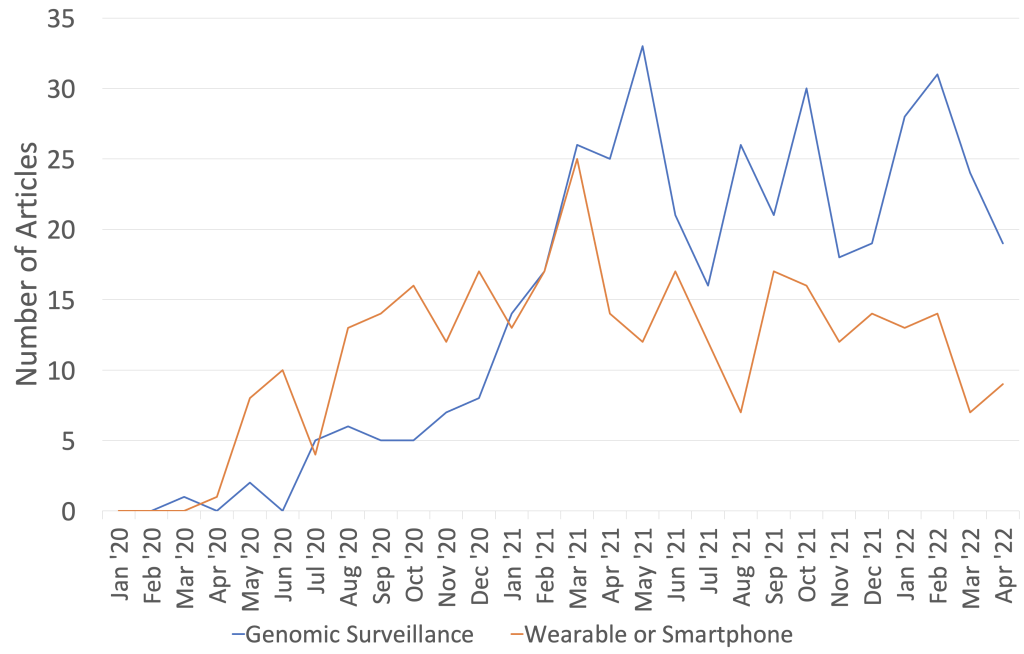
Posted on byTwo recent articles, one in Nature Medicine and another in Nature Biotechnology, highlight areas of health innovation that have been accelerated by the COVID-19 pandemic. This blog post focuses on two precision health applications of technology—(1) genomics and (2) wearable devices and smartphone apps—that are likely to have a lasting impact beyond the pandemic. Increased interest in these applications is reflected in the scientific literature captured by the COVID-19 GPH database (see Figure).
Genomic Surveillance: A Key Tool for Precision Public Health
Genomic surveillance has been at the forefront of the public health response to COVID-19. Scientists have used genetic sequencing of the SARS-CoV-2 genome to track how the virus evolves and spreads in populations. Monitoring the genetic differences that SARS-CoV-2 accrues via mutation has served as an early warning detection system for new viral variants. Some of these are termed variants of concern when evidence suggests that they increase transmissibility or disease severity. Genomic sequencing can also provide insights into transmission and outbreak dynamics. CDC’s Office of Advanced Molecular Detection has developed the COVID-19 Genomic Epidemiology Toolkit, which explains these applications and provides case studies, as well as modules for implementation.
Genomic surveillance is increasingly important in public health efforts to detect and control infectious diseases, by detecting emerging infections and outbreaks, monitoring antimicrobial resistance, and evaluating and improving vaccines.
Wearable Technologies and Smartphone Apps: An Emerging Area for Precision Medicine and Precision Public Health
Advances in sensor and communication technologies have led to development of wearable devices that can monitor and transmit physiological and behavioral data, and smartphone apps that can generate real-time, population-wide data. In contrast to conventional testing (e.g., in a physicians’ office, perhaps several times a year), wearable devices can provide continuous measurements of physical activity and changes in physiological parameters, such as heart rate, body temperature, and blood pressure. Smartphone apps can be used for individual screening with symptoms checkers, allowing users to understand their personalized risk to make informed decisions about their health. Using these tools for long-term monitoring has been proposed for early disease detection, supporting preventative care, and “real-time personalized medicine.”
Wearable sensors can detect and monitor several physiological indicators associated with COVID-19, such as heart rate and respiration rate. For example, a Nature Biomedical Engineering study showed that physiological and physical activity data collected by consumer smartwatches can be used to detect pre-symptomatic cases of COVID-19. Another recent study detected cases of long COVID by comparing wearable sensor data on resting heart rate, sleep, and activity between COVID-19 patients and non-COVID-19 patients. The study found a subset of COVID-19 patients showed elevated heart rates greater than an additional five beats per minute over their baseline for as long as 133 days after symptom onset. With longer duration wearable sensor data, the study uncovered the prolonged physiological impact of SARS-CoV-2 infection lasting 2-3 months on average.
Harnessing wearable and smartphone app data at the population-level can improve real-time disease surveillance, which can refine the precision of public health responses. For example, wearable devices and smartphone apps can be used to inform physical distancing and contact tracing to reduce the likelihood of viral transmission.
Challenges and Next Steps
Genomic surveillance, wearable technology, and smartphone apps have real potential for improving health, but several barriers remain. The continuous processing and storage of large volumes of data and the computational power requirements for analyzing the data is costly.
The security and privacy of user health data must be protected. Securing the confidentiality of health data can foster user trust and ensure equity. The use of wearables in clinical practice will have to be evaluated on a case-by-case basis for its ability to provide clinically useful data that can improve health outcomes. Genomic surveillance, wearable technology, and smartphone apps are emerging tools that will last beyond the COVID-19 pandemic in improving individual and population health.
Posted on by


