Mendelian Randomization: A Precision Public Health Tool for the COVID-19 Response
Posted on by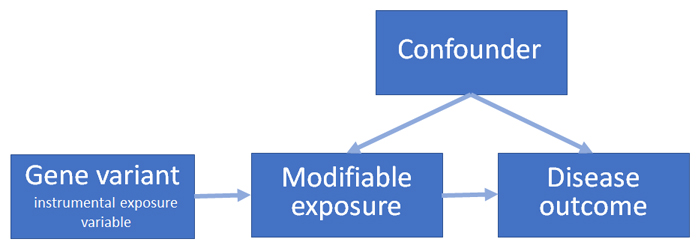 In the early days of the COVID-19 pandemic, when little was known about the natural history of the disease, predicting the course of the pandemic was of premier importance for treating sick patients and redoubling efforts to protect those at highest risk of adverse outcomes. To address this need, investigators used a study design that is rooted in human genetics, Mendelian randomization, an approach that has been used to identify important modifiable risk factors for common chronic diseases.
In the early days of the COVID-19 pandemic, when little was known about the natural history of the disease, predicting the course of the pandemic was of premier importance for treating sick patients and redoubling efforts to protect those at highest risk of adverse outcomes. To address this need, investigators used a study design that is rooted in human genetics, Mendelian randomization, an approach that has been used to identify important modifiable risk factors for common chronic diseases.
Mendelian randomization uses the association of genetic variation with a modifiable exposure and disease outcome as an “instrumental variable” for inferring causal associations between the exposure and the outcome (see figure). This approach minimizes two major concerns with other observational epidemiologic study designs, confounding and reverse causation. Other advantages include requiring less time and expense than conducting a randomized clinical trial, the ability to analyze existing studies, and the ability to address questions that randomized clinical trials are unable to ask.
As of July 14, 2021, 39 Mendelian randomization studies of COVID-19 were available in PubMed. These articles address a variety risk factors for COVID-19 susceptibility and severity (see appendix). For example, one study used Mendelian randomization to analyze 38 traits, including smoking, Alzheimer’s disease, and type 2 diabetes, for association with COVID-19 hospitalization. As an instrumental variable for smoking, the study used single nucleotide polymorphisms (SNPs) found to be related to number of cigarettes smoked per day or smoke inhalation. Using these SNPs as a proxy for smoking, the study found evidence that smoking is associated with a higher risk of hospitalization due to COVID-19. Four other Mendelian randomization studies have also provided evidence for a causal association between smoking and COVID-19 outcomes.
Obesity was identified early on as a potential risk factor for COVID-19 severity. However, obesity is also associated with other conditions, such as hypertension and type 2 diabetes, that could confound its association with COVID-19. A recent study of hospitalization for COVID-19 used genetic variants associated with body mass index (BMI) or waist circumference as instrumental variables for obesity. The results supported the inference that obesity is a risk factor for severe COVID-19. Six other Mendelian randomization studies also supported a causal association between BMI and COVID-19 outcomes.
Biochemical indices have also been studied for association with COVID-19 using Mendelian randomization. A recent study using SNPs related to either vitamin D serum levels or disposition to vitamin D deficiency provided evidence against vitamin D status as a protective factor for COVID-19 susceptibility or severity. Three other independent Mendelian randomization studies have supported this conclusion.
Mendelian randomization studies have also been designed to suggest possible treatments for COVID-19. One study provided evidence for IFNAR2 and ACE2 levels as possible drug targets. Another study used Mendelian randomization to suggest existing drugs with potential for repurposing as COVID-19 treatments. Such results can be used to prioritize drugs for further investigation in observational studies or randomized clinical trials.
Mendelian randomization studies have grown in popularity in the past two decades. In 2010, there were 61 published articles in PubMed while in 2020, there were 892 articles. They have evolved from focusing on environmental exposures to investigating disease processes and potential drug treatments. Like other epidemiologic methods, Mendelian randomization has its own limitations such as a lack of genetic variants as proxies of the modifiable exposure, confounding due to population stratification, and variable effects of genetic variants on outcomes. In general, using a combination of study designs, with different strengths and weaknesses, increases the strength and validity of scientific evidence of the relationship between exposures and disease outcomes. The contributions of Mendelian randomization are likely to continue to evolve as a way to use human genomics to uncover modifiable causes of human disease.
Appendix: Mendelian randomization and COVID-19 articles in PubMed as of July 14, 2021
| PubMed ID | Author | Category and Risk Factors of Interest | COVID-19 Outcomes | Conclusion |
|---|---|---|---|---|
| 33349849 | Butler-Laporte G, et al. | Biochemical levels | Genetically proxied lower serum-ACE levels was not associated with COVID-19 susceptibility. | A lower serum-ACE levels do not increase an individual’s risk for contracting COVID-19. |
| 33307546 | Pairo-Castineira E, et al. | Biochemical Levels | Genetically proxied low expression of IFNAR2, high expression of TYK2 are associated with life-threatening COVID-19 disease while high expression of CCR2 was associated with severe COVID-19 disease. | IFNAR2, TUK2, CCR2 levels might be drug targets for COVID-19. |
| 33633408 | Zhou S, et al. | Biochemical Levels | Genetically proxied increase in OAS1 levels were associated with reduced risk for COVID-19 death, ventilation, hospitalization, and susceptibility. | Higher OAS1 levels might be protective against poor COVID-19 outcomes. |
| 33445938 | Kopecek M, et al. | Biochemical levels | Genetically proxied serum vitamin D levels were not associated with COVID-19 infection. | Vitamin D serum levels might not be a risk factor for COVID-19 infection. |
| 34061844 | Butler-Laporte G, et al. | Biochemical levels | Genetically proxied higher 25OHD levels were not associated with COVID-19 infection, hospitalization, or severity. | Vitamin D levels might not be a risk factor for COVID-19 infection, hospitalization, or severity. |
| 34246301 | Cui Z, et al. | Biochemical Levels | Genetically proxied serum 25OHD concentration was not associated with COVID-19 susceptibility, severity, or hospitalization. | Vitamin D supplementation might not be helpful against COVID-19. |
| 33548839 | Richardson T, et al. | Cardiometabolic Factors | Genetically proxied glycoprotein 130 was associated with severe COVID-19. | Glycoprotein 130 might be an important factor to further research for COVID-19 severity. |
| 33757497 | An Yeung S, et al. | Cardiometabolic Factors | Genetic liability to type 2 diabetes and glycemic traits were not associated with COVID-19 outcomes. | Type 2 diabetes and poorer glycemic traits are not associated with increased risk for COVID-19. |
| 33846372 | Lorincz-Comi N, et al. | Cardiometabolic Factors | Genetic liability to type 2 diabetes and genetically proxied pulse pressure were not associated to COVID-19 hospitalization. | Type 2 diabetes and pulse pressure might not be risk factors for COVID-19 hospitalization. |
| 33667465 | Hilser J, et al. | Cardiometabolic Factors | Genetically proxied higher HDL-cholesterol levels were not associated with decreased risk COVID-19 susceptibility and mortality. | Higher HDL cholesterol level might not be protective against COVID-19 infection and susceptibility. |
| 33262790 | Aung N, et al. | Cardiometabolic Factors | Genetically proxied higher BMI and LDL cholesterol were associated with susceptibility to COVID-19. WC, SBO, serum glucose, HbA1c, HDL and triglycerides were not associated with susceptibility to COVID-19. | Obesity and a higher LDL cholesterol level might be risk factors for COVID-19 infection. |
| 32909013 | Leong A, et al. | Cardiometabolic Factors | Genetically proxied increased BMI was associated with COVID-19 infection and severity. | Higher BMI might be a risk factor for COVID-19 susceptibility and severity. |
| 33661905 | Leong A, et al. | Cardiometabolic factors | Genetically proxied BMI was associated with COVID-19 severity. Genetically higher BMI was not associated with a higher risk for testing positive for COVID-19 but was associated with COVID-19 hospitalization | Higher BMI is a risk factor for COVID-19 hospitalization, severity, but not susceptibility. |
| 33631142 | Freuer D, et al. | Cardiometabolic Factors | Genetically proxied BMI was associated with COVID-19 susceptibility and hospitalization. | Obesity is associated with COVID-19 susceptibility and severity. |
| 34202464 | Wang M, et al. | Cardiovascular | Genetically proxied blood pressure was associated with severe COVID-19 with respiratory failure. | Blood pressure might be a risk factor for severe COVID-19 with respiratory failure. |
| 34127963 | Roh J, et al. | Cardiovascular | In COVID-19 patients, genetically proxied ADAMTS13 was associated with myocardial injury. | ADAMTS13 might be a risk factor for myocardial injury in COVID-19 patients. |
| 33837377 | Gaziano L, et al. | Drugs | The ACE2, IFNAR2, and IL-10RB proteins were associated with COVID-19 hospitalization. | ACE2 and IFNAR2 might be drug targets for COVID-19 |
| 34163532 | Li M, et al. | Immune System | Higher chemokine (C-C motif) ligands 4 levels were associated with lower risk for COVID-19 hospitalization. | Chemokine (C-C motif) ligands 4 might be an important immune response element to further research for COVID-19. |
| 33809027 | Sun Y, et al. | Immune System | Higher basophil count, basophil percentage of WBC, myeloid WBC were associated with lower risk for severe COVID-19. Basophil count, basophil percentage of WBC, and myeloid WBC were not associated with COVID-19 susceptibility. | White blood cell traits are associated with COVID-19 severity but not with COVID-19 susceptibility. |
| 34189540 | Zhang S, et al. | Immune System | Genetically proxied failure of natural killer cell NKG2D-mediated activation was associated with severe COVID-19. | Natural killer cell function might be risk factor for severe COVID-19. |
| 33214204 | Larsson S, et al. | Immune System | Genetically proxied IL6R inhibition was associated with lower risk of COVID-19 susceptibility and hospitalization. | IL6R inhibition may be protective against COVID-19 infection and hospitalization. |
| 33312507 | Zhang X, et al. | Lifestyle Factors | Genetically proxied moderate to vigorous physical activity was not associated with COVID-19 outcomes. | Moderate to vigorous physical activity might not be protective or a risk factor for COVID-19. |
| 33269370 | Fan X, et al. | Lifestyle factors | Genetically proxied binary, four-level categorical, and continuous alcohol consumption were not associated with COVID-19 susceptibility. Genetically proxied higher alcohol consumption was associated with a higher risk of death from COVID-19 in obese patients but not in non-obese patients. | Higher alcohol consumption is associated with a higher risk of COVID-19 related death in obese patients. |
| 34227468 | Liu H, et al. | Lifestyle Factors | Genetically proxied smoking was associated with ACE2 expression. Genetically proxied alcohol consumption was not associated with ACE2 expression. | Smoking, but not alcohol consumption, might be a risk factor for increased ACE2 expression and therefore affect COVID-19 susceptibility. |
| 34150709 | Yoshikawa M, et al. | Lifestyle Factors | Genetically proxied higher educational attainment was associated with a lower risk for severe COVID-19 | Higher educational attainment might be protective for COVID-19. |
| 33833219 | Luykx J, et al. | Psychiatric Disorders | Genetic liability to schizophrenia and Alzheimer’s disease was associated to COVID-19 susceptibility. Genetic liability to schizophrenia and bipolar disorder were associated with severe COVID-19. | Psychiatric disorders such as schizophrenia, Alzheimer’s disease, and bipolar disorder might be associated with COVID-19 severity or susceptibility. |
| 33714028 | Fadista J, et al. | Respiratory | Genetically disposed idiopathic pulmonary fibrosis was associated with increased risk for severe COVID-19. | Idiopathic pulmonary fibrosis might be a risk factor for severe COVID-19. |
| 33391794 | Gill D, et al. | Drugs, Biochemical Levels | There was no association between genetically proxied serum ACE2 levels and COVID-19 hospitalization | Serum ACE2 levels may not be a risk factor for COVID-19 and therefore, may not be an effective drug target. |
| 34099622 | Zhou Y, et al. | Biochemical Levels, Immune System | Genetically proxied VWF, VWF activity, and ADAMTS13 were associated with COVID-19 severity. | VWF and ADAMTS13 might be important factors for COVID-19 severity. |
| 33822963 | Ran S, et al. | Cardiometabolic Factors, Immune System | Genetically proxied COVID-19 was associated with lower eosinophil cell levels and LDL cholesterol. | COVID-19 might be a risk factor for low eosinophil cell and LDL cholesterol levels. |
| 32966752 | Ponsford M, et al. | Cardiometabolic Factors, Lifestyle Factors | Genetically proxied lifetime smoking and higher BMI were associated with increased risk of severe COVID-19, COVID-19 hospitalization, and COVID-19 respiratory failure. | Smoking and BMI might be risk factors for COVID-19 severity, hospitalization, and respiratory failure. |
| 33536004 | Li S, et al. | Cardiometabolic Factors, Lifestyle Factors | Genetically proxied smoking and higher BMI were associated with increased risk for COVID-19 hospitalization and severity. Genetically proxied physical activity was associated with a lower risk for COVID-19 severity. | Smoking and higher BMI are associated with increased risk for COVID-19 severity and hospitalization. Physical activity is associated with lower risk for COVID-19 severity. |
| 33259846 | Liu D, et al. | Cardiovascular,
Respiratory |
Genetically proxied ILMN_1765156 and ILMN_1791057 probes for IFNAR2 were associated with COVID-19 hospitalization. | IFNAR2 might be risk factors for COVID-19 hospitalization. |
| 33604698 | Hernandez A, et al. | Cardiovascular, Respiratory | Genetically proxied plasma ABO protein was associated with an increased risk for severe COVID-19. | Plasma ABO protein might be a risk factor for COVID-19. |
| 33594380 | Rosoff D, et al. | Lifestyle factors, Respiratory | Genetically proxied smoking was associated with increased risk for COVID-19 hospitalization and severe hospitalization. | Smoking might be a risk factor for COVID-19 hospitalization. |
| 34122505 | Wang K, et al. | Biochemical Levels, Cardiovascular, Immune System | A higher neutrophil, monocyte, and lymphocyte counts were associated with a lower risk for COVID-19. | Higher white blood cell counts might be protective for severe COVID-19. |
| 32430459 | Rao S, et al. | Cardiometabolic Factors, Cardiovascular, Drugs | Genetic liability to type 2 diabetes was associated with increased ACE2 expression | Drug treatments for type 2 diabetes might be possible drugs for managing ACE2 expression. |
| 33688662 | Zuber V, et al. | Cardiometabolic Factors, Cardiovascular, Lifestyle Factors | Genetic liability to COVID-19 was associated with an increased risk of ischemic stroke. Genetic liability to ischemic stroke was not associated to severe COVID-19. | COVID-19 might be associated with an increased risk for ischemic stroke but ischemic stroke might not be a risk factor for severe COVID-19. |
| 34237774 | COVID-19 Host Genomics Initiative | Cardiometabolic Factors, Biochemical Levels, Lifestyle Factors, Cardiovascular, Respiratory, Psychiatric Disorders | Genetically proxied smoking and BMI were associated with severe COVID-19. Genetically liable type 2 diabetes was not associated with severe COVID-19. | Smoking and BMI might be risk factors for severe COVID-19. Type 2 diabetes might not be a risk factor for severe COVID-19. |
25-hydroxybitamin D (25OHD), angiotensin-converting enzyme 2 (ACE2), a disintegrin and metalloproteinase with a thrombospondin type I motif, member 13 (ADAMTS13), body mass index (BMI), C-C motif chemokine receptor 2 (CCR2), serum glycated hemoglobin (HbA1c), high density lipoproteins (HDL), interferon alpha and beta receptor subunit 2 (IFNAR2), interleukin 10 receptor subunit beta (IL-10RB), interleukin 6 receptor (IL6R), natural killer group 2, member D (NKG2D), oligoadenylate synthetase 1 (OAS1), systolic blood pressure (SBO), tyrosine kinase 2 (TYK2), low density lipoproteins (LDL), von Willebrand factor (VWF), white blood cell (WBC), waist circumference (WC),
Posted on by


