Personal Reflections on Genomics, Health Equity, and Public Health
Posted on by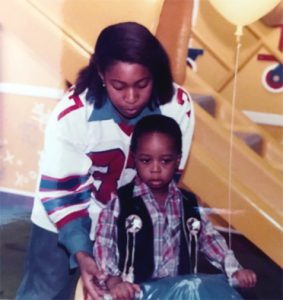 My nephew, Eddie, and niece, Sheri, were lively, witty, high-spirited, active, bright, and full of hope. Eddie dreamed of becoming a professional baseball player, while Sheri aspired to become a mathematical engineer. But their childhood diagnoses with a type of kidney disease called nephrotic syndrome ended those dreams. While nephrotic syndrome can be inherited, we had never heard of anyone else in our family who had it. Despite receiving treatment for nephrotic syndrome at a leading medical teaching institution, Eddie died 5 days after turning 24, three years after a rejected kidney transplant, and Sheri died just before her 31st birthday, while awaiting a kidney transplant.
My nephew, Eddie, and niece, Sheri, were lively, witty, high-spirited, active, bright, and full of hope. Eddie dreamed of becoming a professional baseball player, while Sheri aspired to become a mathematical engineer. But their childhood diagnoses with a type of kidney disease called nephrotic syndrome ended those dreams. While nephrotic syndrome can be inherited, we had never heard of anyone else in our family who had it. Despite receiving treatment for nephrotic syndrome at a leading medical teaching institution, Eddie died 5 days after turning 24, three years after a rejected kidney transplant, and Sheri died just before her 31st birthday, while awaiting a kidney transplant.
We now know more about nephrotic syndrome than we did back in the 1990s when Eddie and Sheri were diagnosed. Children with nephrotic syndrome have kidney damage that causes them to pass too much of a protein called albumin in their urine. They also can have low amounts of protein in their blood, swelling in different parts of their body, weight gain, less urine, and high cholesterol. While most forms of nephrotic syndrome are idiopathic, meaning that the cause is unknown, some are inherited, meaning that they have a genetic cause. Studies of familial cases have identified both autosomal dominant and recessive forms and have led to the discovery of at least seven genes associated with inherited nephrotic syndrome. Studies in the U.S. have found higher rates of nephrotic syndrome in children of African descent, compared with children of European descent.
 Genomics provides opportunities to prevent, treat, or manage diseases by identifying genetic changes before signs or symptoms of disease occur. But not everyone receives the benefits provided by genomics, and some have even claimed that genomics might widen health disparities among some racial and ethnic minority groups. For example, studies have found lower rates of BRCA genetic counseling and testing among racial and ethnic minority groups. A greater understanding of the role of genetics in chronic conditions might be pivotal for increasing use of genetic counseling and testing for these conditions among some racial and ethnic minority groups.
Genomics provides opportunities to prevent, treat, or manage diseases by identifying genetic changes before signs or symptoms of disease occur. But not everyone receives the benefits provided by genomics, and some have even claimed that genomics might widen health disparities among some racial and ethnic minority groups. For example, studies have found lower rates of BRCA genetic counseling and testing among racial and ethnic minority groups. A greater understanding of the role of genetics in chronic conditions might be pivotal for increasing use of genetic counseling and testing for these conditions among some racial and ethnic minority groups.
What can public health genomics learn from public health work to address health inequities, which focuses on eliminating disparities in health and health care? As a health scientist working to address health inequities, I have found that inequities can relate to timely access to health information needed to obtain leading-edge health care and services. If we are to address health equity in genomics, we need to increase awareness and knowledge, for example among racial and ethnic minority groups who are at risk for specific diseases. To do that, we must engage communities and empower individuals to gain greater knowledge about health conditions.
Some of the approaches used by CDC in the past could be applied to genomics. For example, as part of the 2007 “Breaking the Silence: Church Conversations about HIV/AIDS” initiative, CDC engaged the faith sector and provided a series of conferences that were used as forums to bring people together to share information about public health issues and to collaborate toward addressing those issues. CDC created “A Pastor’s Guide,” which included answers to questions about HIV/AIDS and resources tailored to each community. African American pastors have significant influence within their congregations and play key roles in the health of their communities. Consequently, partnering with the faith community helped to extend the reach of information sharing, and the initiative succeeded in increasing engagement of several faith leaders in developing and supporting programs to fight HIV. Genomics could address health equity by replicating such community engagement strategies for topics such as family health history or specific hereditary conditions, for example, hereditary breast and ovarian cancer, Lynch syndrome, or familial hypercholesterolemia.
Nephrotic syndrome is one of many health conditions for which health inequities exist. We have learned so much since Eddie and Sheri passed, and I wonder if their outcomes might have been different if they had been diagnosed today. Would genetic testing have helped them? We now know that among African Americans with nephrotic syndrome, certain variants of the gene APOL1 increase the likelihood of developing focal segmental glomerulosclerosis and progressing to end-stage renal disease. Could their care have been managed differently? Eddie received his kidney transplant from his father. Research has found that kidney donations from family members might increase the risk for end-stage renal disease in the transplanted kidney, possibly due to shared genetic risk. Knowing this information is not enough, though. Public health work on health equity shows us that we need to make sure that this information reaches those who need it—and provides us with approaches that we might consider trying.
Posted on by


