Public Health is Striving Towards More Precision
Posted on by In the past few years, the term “precision medicine” has become firmly established in the modern biomedical research enterprise. More recently, the term “precision” has made its way to the realm of public health. We and others have contributed to the discourse on precision public health and its relation to precision medicine. But not everyone agrees that the term “precision” should be applied to public health. There is still ongoing concern that the discourse about “precision” in public health still puts too much emphasis on genomics and on individual level interventions, rather than the underlying structural, social and environmental determinants of health. We are excited about the prospects that new technologies can move public health towards more “precision,” and would like to continue to promote conversations on the definitions and scopes of precision medicine and precision public health.
In the past few years, the term “precision medicine” has become firmly established in the modern biomedical research enterprise. More recently, the term “precision” has made its way to the realm of public health. We and others have contributed to the discourse on precision public health and its relation to precision medicine. But not everyone agrees that the term “precision” should be applied to public health. There is still ongoing concern that the discourse about “precision” in public health still puts too much emphasis on genomics and on individual level interventions, rather than the underlying structural, social and environmental determinants of health. We are excited about the prospects that new technologies can move public health towards more “precision,” and would like to continue to promote conversations on the definitions and scopes of precision medicine and precision public health.
Precision medicine starts with the individual. Precision medicine may have had firm roots in the genomics movement, and more recently other ‘omic’ fields, and big data, more broadly defined. But a more comprehensive approach is firmly embedded in the All of US Research Program. The term precision medicine encompasses both treatment and prevention, genes, environments and social factors. “Precision medicine is a revolutionary approach for disease prevention and treatment that takes into account individual differences in lifestyle, environment, and biology.” There is a common notion that precision necessarily implies biologic determinism, primarily in the use of genetic information. While this may be true for certain conditions, most human diseases are due to complex gene-environment interactions which can only lead to a probabilistic (albeit more precise) approach to treatment and prevention.
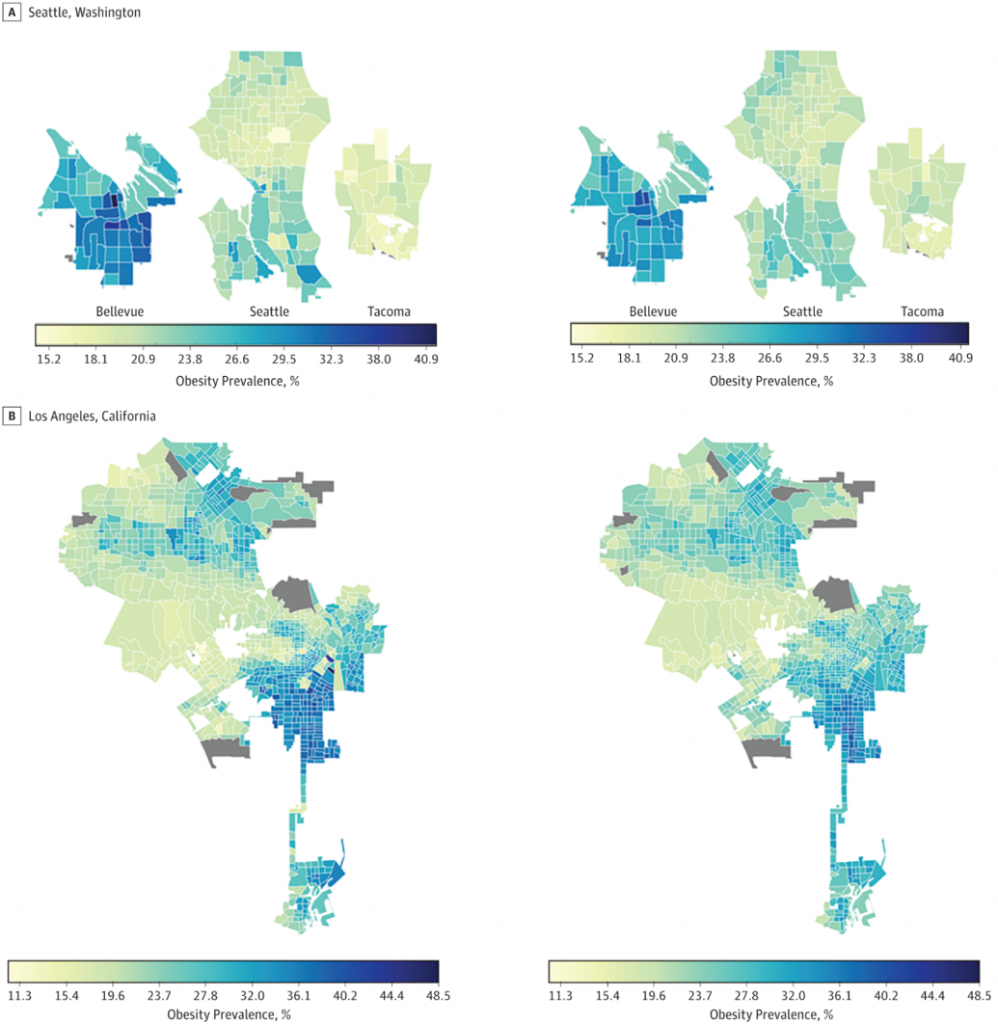
Precision public health begins with populations. Many factors affecting the health of populations have no individual-level interventions but can respond better to social, environmental and policy changes, if we can identify them with more precision. Public health also uses clinical interventions at the individual level as one approach to improving health and reduce health disparities; within that approach, genomics is only one component. Population health assessment is essential to develop the right health policies, whether or not they lead to individual interventions. The same tools and technologies that currently fuel the precision medicine movement may help produce more precision in the public health functions of assessment, policy development and ensuring health and dealing with health inequity. In our 2016 paper, we gave several examples of areas of potential growth in precision public health, including enhanced public health surveillance, targeted public health interventions, and the use of technologies in the public health investigations and control of infectious diseases. A more recent example of how new tools and technologies are providing approaches to assessing population health problems is the JAMA Network Open article that used deep learning to examine the association of the built environment with the prevalence of neighborhood adult obesity. In this modeling study of four U.S. urban areas, extraction of built environment information from more than 100,000 space images using convolutional neural networks to assess associations between the built environment and obesity prevalence. The study showed that physical characteristics of a neighborhood (eg, the presence of parks, highways, green streets, crosswalks, diverse housing types) can be associated with variations in obesity prevalence across different neighborhoods. As shown in the figure, note on the left the actual obesity rates in high obesity areas in Seattle and Los Angeles. Compare the observed obesity rates with the predicted rates as essentially spotted from space on the right hand. A remarkable similarity. The same pattern was seen in low obesity areas (not shown here). This is what prompted the caption in one news media coverage about “Artificial intelligence spotting obesity from space.”
As the previous example shows, precision public health is not just about genomics and disease treatment at the individual level. While some are concerned that the field has rarely addressed social and environmental determinants of health, the focus on social, economic and health disparities, has been part and parcel of the dialogue that occurred at the 2016 UCSF precision public health summit, and is firmly embedded in the 2018 precision public health Asia meeting.
It is time for public health to evaluate the utility of emerging technologies to enhance the precision of its impact. Advances in data storage and linkages, digital technologies, computational power, genetic, epigenetic and other ‘omic’ data, geographic information, environmental exposure data will, over time, help improve population health assessments, reconciling and combining the influence of biological and social factors on disease occurrence, leading to better population and individual level interventions and approaches to remedy health inequities.
Medicine is striving towards more precision. I believe, public health practice is also striving towards more precision. But let’s not throw out the baby with the bath water. The word “precision” should not stand in the way of better collaboration between medicine and public health in using emerging technologies to improve health for all.
Posted on by


