Manipulating the Human Microbiome for Precision Public Health: Prospects and Challenges
Posted on bySpotlight on the Human Microbiome
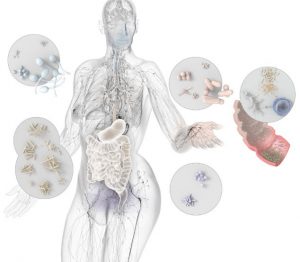
The human microbiome has a crucial role in driving public health science and initiatives towards more “precision”.
In a recent viewpoint and podcast, Harkins, et al. discuss the potential and current applications for manipulating the human microbiome for disease prevention and management. The authors describe several examples of microbiome manipulation as promising novel therapies. Harkins, et al. highlight a recent, large randomized controlled trial demonstrating the ability of a probiotic and prebiotic supplement to prevent neonatal sepsis among children in India. In addition, fecal microbiota transplantation (FMT), representing administration of feces, a live biotherapeutic, is increasingly applied in the management of multiply recurrent Clostridioides difficile infection (CDI), even as the function of the human microbiome in prevention of CDI is still studied. Despite these advances, manipulating complex microbial communities for a particular outcome still presents challenges. Harkins, et al. note the need for more understanding of the relationship between the microbiome and inflammatory bowel disease pathogenesis. They conclude by summarizing how challenges in manipulating human microbiomes are dependent upon the complexity of the usual microbiota at a particular body site, the importance of specific strain functions, and understanding the role of microbiota in pathogenesis.
Progress in understanding how the human microbiome can be leveraged for public health is exemplified in a recent CDC-funded study. Robinson, et al. explored the relationship between the intestinal metabolome (all chemicals present in the intestine) and CDI through fecal metabolomic profiling. The authors identified metabolites and metabolic processes correlated with CDI pathogenesis and suggested novel diagnostic approaches for CDI utilizing metabolomic profiles rather than traditional diagnostic approaches.
Another area of CDC-funded research involves identifying intermediate milestones of antibiotic-mediated microbiome disruption which may provide data for action that leads to reductions in transmission of multidrug-resistant organisms, infection, and even sepsis. Shimasaki, et al. found an association between high levels of carbapenem-resistant Klebsiella pneumoniae in the gut microbiome and an increased risk of bacteremia, suggesting either bacterial translocation from the gut into the bloodstream or a tendency for this dominant state to lead to skin contamination resulting in catheter-associated bacteremia. Similarly, Pettigrew, et al. found that, due to ongoing antibiotic treatment, the majority of their patients in intensive care units had dominance of their gut microbiome by potential pathogens. Together these studies provide insights into the observations in another study conducted by CDC scientists in which Baggs, et al. identified dose-response associations between receipt of antibiotics during hospitalization and subsequent re-admission for sepsis.
Simpler Microbiomes Offer an Opportunity for More Rapid Progress towards Precision Health
The above publications exemplify what Harkins et al. described as the considerable challenges of working with a complex microbiome, such as the GI microbiome; body sites reflecting a simpler aspect of the human microbiome may offer greater opportunity for rapid progress. For the normally less diverse vaginal microbiome, live biotherapeutics are under development to treat bacterial vaginosis, a disorder associated with increased diversity and loss of the normal, healthy mono-dominance by Lactobacillus spp. In another example of CDC-funded work with a simpler human microbiome, Dr. Sam Brown’s lab at Georgia Tech is examining the microbiota in the lungs of cystic fibrosis patients to better understand these microbial communities and subsequently tailor antibiotic treatment to the patient and their specificdisease state.
Regardless of the body site, individualized treatment strategies across human microbiomes may be able to enhance treatment effectiveness, improve antibiotic stewardship, and reduce resistance.
CDC in Action
Looking forward, the National Center for Emerging and Zoonotic Diseases will continue to fund research, collaborate across the agency, and engage external stakeholders to increase understanding of the microbiome for precision public health. We are initiating cross-Agency dialogue on the relevance of the human microbiome in multiple areas, such as diagnostics for infectious and chronic diseases, and further evaluating the role of the microbiome in public health surveillance, research, and prevention.
Definitions:
Live biotherapeutic: A biological product that:
1) contains live organisms, such as bacteria
2) is applicable to the prevention, treatment, or cure of a disease or condition of human beings
3) is not a vaccine (FDA PDF 174KB)
Prebiotics: Nondigestible food components that selectively stimulate the growth or activity of desirable microorganisms (NIH)
Probiotics: Live microorganisms which when administered in adequate amounts confer a health benefit on the host (WHO PDF 54.2KB)
Posted on by


