Safe Healthcare Blog
Infection control reminders during this challenging respiratory virus season

Abigail L. Carlson, MD, MPH, Physician, Project Firstline, Division of Healthcare Quality Promotion, CDC With assistance from Mia Frederick (contractor, TANAQ) a writer for CDC’s Project Firstline in the Division of Healthcare Quality Promotion. Over the past few months, there has been an increase in respiratory virus activity nationwide, causing additional strain on an already Read More >
Posted on by 5 Comments“I’m Concerned About Sepsis!”

This blog is a part of a series that CDC launched to highlight the importance of patient safety by providing educational information and simple ways to help people stay informed on public safety topics. Read the blog below, authored by Dr. Carl Flatley, to learn more about sepsis and the importance of voicing your concerns Read More >
Posted on by 1 CommentAsking Your Healthcare Provider the Hard Questions
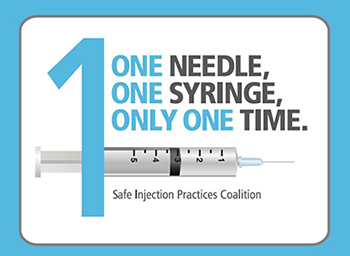
This blog is a part of a series that CDC launched to highlight the importance of patient safety by providing educational information and simple ways to help people stay informed on public safety topics. Read the blog below, authored by Evelyn McKnight, to learn more about preventing unsafe injection practices. When I was diagnosed with Read More >
Posted on by 4 CommentsSeeing The Potential Harm of Antibiotic Overuse Clearly

This blog is a part of a series that CDC launched to highlight the importance of patient safety by providing educational information and simple ways to help people stay informed on public safety topics. Read the blog below, authored by Christian John Lillis, to learn more about the potential harms of antibiotic overuse. The widespread Read More >
Posted on by 2 CommentsFrom Unaware and Unprepared to Safe Healthcare Advocates

This blog is a part of a series that CDC launched to highlight the importance of patient safety by providing educational information and simple ways to help people stay informed on public safety topics. Read the blog below, authored by Nile’s Project founders Carole and Ty Moss, to learn more about the importance of preventing Read More >
Posted on by 7 Comments

