Addressing Racial and Ethnic Health Disparities in Adult Obesity and Encouraging Physical Activity this National Minority Health Month
Posted on byEvery person should be able to reach his or her full health potential. I’m proud of the work we do in CDC’s Division of Nutrition, Physical Activity, and Obesity (DNPAO) to support Americans’ journey to good health—especially among people most vulnerable to chronic disease. We protect the health of Americans at every stage of life by encouraging regular physical activity and good nutrition, helping to prevent obesity in children and adults, and addressing barriers to treating obesity in children.
Obesity is a serious health problem and the prevalence of obesity continues to increase among adults in the United States. We know that obesity is common, serious, and costly. This epidemic is putting a strain on American families, affecting individuals’ overall health, health care costs, productivity, and military readiness. We also know that obesity affects some groups more than others. To be successful, we must reduce racial and ethnic disparities in obesity.
Here I’m going to discuss the costs of obesity and how it is disproportionally affecting some racial and ethnic groups more than others. I’m also going to talk about physical activity as one of the strategies we promote to address obesity. Finally, I’ll share how CDC’s Racial and Ethnic Approaches to Community Health (REACH) program, State Physical Activity and Nutrition Program (SPAN), and High Obesity Program (HOP) are working with communities to improve physical activity access, among other strategies, to help people most at risk for chronic disease.
Costs of Obesity
Obesity is a problem for both children and adults in the United States. Nearly 1 in 5 young people aged 2 to 19 years have obesity. These children are at risk for type 2 diabetes, asthma, depression, and low self-esteem. The risk of adult obesity is also increased for individuals who had obesity as children.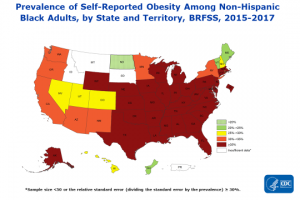
Nearly 4 in 10 adults in the United States have obesity. Adults with obesity often have multiple-organ system complications from the condition and are more at risk for heart disease, stroke, type 2 diabetes, and 13 types of cancers. Obesity costs the US health care system approximately $147 billion a year. Adult obesity decreases productivity and increases the risk of workplace injuries. The cost of obesity-related absenteeism is between $3.4 billion and $6.4 billion each year. Obesity in young adults limits the eligibility for many to serve in our military. About 1 in 4 young adults is too heavy to serve.
Disparities
CDC plays a key role in tracking data on obesity burden and the racial and ethnic disparities within the obesity burden. Using self-reported data from the Behavioral Risk Factor Surveillance System (BRFSS), we have published state obesity maps since 1999. For the past 4 years, we published more detailed state and territorial maps to show self-reported adult obesity by race/ethnicity to bring awareness to the disparities in obesity.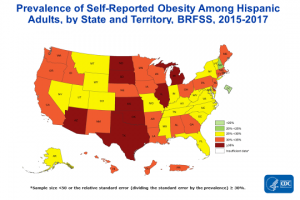
The racial and ethnic maps for 2015–2017 show where obesity is more burdensome for particular populations. Overall, 31 states and the District of Columbia had an obesity prevalence of 35% or higher among non-Hispanic black adults; 8 states (Arizona, Illinois, Kansas, Michigan, North Dakota, Oklahoma, South Dakota, and Texas) had an obesity prevalence of 35% or higher among Hispanic adults; and only 1 state (West Virginia) had an obesity prevalence of 35% or higher among non-Hispanic white adults.
Encouraging Physical Activity to Manage and Prevent Obesity
There is no single or simple solution to the obesity problem our nation faces. We do know there are proven strategies to help turn this around if we work together and across sectors. In the spirit of the 2019 National Minority Health Month’s Active & Healthy theme, I would like to talk about one strategy—increasing physical activity. Physical activity, when combined with a healthy diet, can help people prevent unhealthy weight gain and help them lose weight.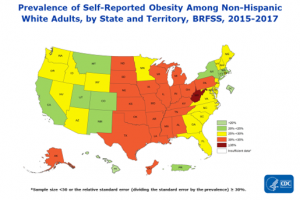
However, physical activity has many other benefits beyond helping with weight management. Physical activity promotes health by reducing the risk of chronic diseases and other conditions that are often more common and more severe among racial and ethnic minority groups. Physical activity also fosters normal growth and development in children, improves mental health, and can make people feel better, function better, and sleep better. The Physical Activity Guidelines for Americans outlines the amounts and types of physical activity needed to maintain or improve overall health and reduce the risk of chronic disease.
Despite the benefits of physical activity, too few Americans get the recommended amount of physical activity. Only 1 in 4 adults and 1 in 5 high school students fully meet physical activity guidelines for aerobic and muscle-strengthening activities. These numbers are even lower among adults in some racial and ethnic minority populations.
One way communities can help residents be active is to create easy and safe options for physical activity. Since 1999, CDC’s Racial and Ethnic Approaches to Community Health (REACH) program has demonstrated that through community participation, locally-based and culturally-tailored efforts can be effective. REACH communities address chronic diseases for specific racial and ethnic groups in urban, rural, and tribal communities with high disease burden. They implement community planning and transportation plans that support safe and accessible physical activity by connecting sidewalks, paths, bike routes, and public transit with homes, early care and education settings, schools, and parks and recreation centers.
CDC’s State Physical Activity and Nutrition Program (SPAN) and High Obesity Program (HOP) also focus on improving racial and ethnic health disparities and include strategies to increase physical activity. Through SPAN, CDC funds statewide initiatives to implement evidence-based strategies at state and local levels to improve nutrition and physical activity. CDC’s HOP funds 15 land grant universities to work with community extension services to increase access to healthier foods and safe and accessible places for physical activity in counties that have more than 40% of adults with obesity.
Visit DNPAO’s website for more information on why physical activity matters, what your community can do to become more activity-friendly, and how you can work with Active People, Healthy Nation to help 27 million Americans become more physically active by 2027.
Together, we can help states and communities to improve physical activity access and to reduce obesity rates for all Americans.



Post a Comment