Mission Possible: Treat Me Right
Posted on by
In the fall of 1999, in preparation for the launch of The National Plan to Eliminate Syphilis from the United States, I was asked to draft a letter to the survivors of the U.S. Public Health Service Tuskegee Study of Untreated Syphilis in the Negro Male, or the Tuskegee Study as it is usually called. The letter would inform the men about the new program. It was two years after the historic Presidential Apology for the infamous syph ilis study, and leadership in the Division of STD Prevention desired to demonstrate our commitment to eliminating a scourge that has persisted in the U.S., particularly among those who are the most disadvantaged in our society. Those were heady days in September of 1999. Many of us were optimistic, confident that our mission to eliminate syphilis was possible.1 Infectious syphilis cases had never been lower since official reporting began. We had the silver bullet of penicillin and a health department-based delivery system. So sure of our success, we believed that once we eliminated syphilis we could turn our attention and our tools to the prevention and control of other STDs like gonorrhea and chlamydia. Reducing the racial/ethnic STD disparities in the U.S. by beginning with syphilis was deemed a fitting tribute to the men who had been so badly abused by the notorious Tuskegee Study. Ultimately the letter was not sent because others advised against it, arguing that such a letter would link this latest syphilis elimination effort to the infamous study, as if history had not already done this.
ilis study, and leadership in the Division of STD Prevention desired to demonstrate our commitment to eliminating a scourge that has persisted in the U.S., particularly among those who are the most disadvantaged in our society. Those were heady days in September of 1999. Many of us were optimistic, confident that our mission to eliminate syphilis was possible.1 Infectious syphilis cases had never been lower since official reporting began. We had the silver bullet of penicillin and a health department-based delivery system. So sure of our success, we believed that once we eliminated syphilis we could turn our attention and our tools to the prevention and control of other STDs like gonorrhea and chlamydia. Reducing the racial/ethnic STD disparities in the U.S. by beginning with syphilis was deemed a fitting tribute to the men who had been so badly abused by the notorious Tuskegee Study. Ultimately the letter was not sent because others advised against it, arguing that such a letter would link this latest syphilis elimination effort to the infamous study, as if history had not already done this.
 Now, nearly twenty years later, it is STD Awareness month the theme of which is: Treat Me Right. Looking into the prominently featured young faces of mostly minority persons on the Division of STD Prevention website I am reminded of the African American men from the syphilis study. They, too, had been young and members of communities disproportionately burdened by STDs. I can imagine them making the request of the doctors and nurses they encountered: Treat me right.
Now, nearly twenty years later, it is STD Awareness month the theme of which is: Treat Me Right. Looking into the prominently featured young faces of mostly minority persons on the Division of STD Prevention website I am reminded of the African American men from the syphilis study. They, too, had been young and members of communities disproportionately burdened by STDs. I can imagine them making the request of the doctors and nurses they encountered: Treat me right.
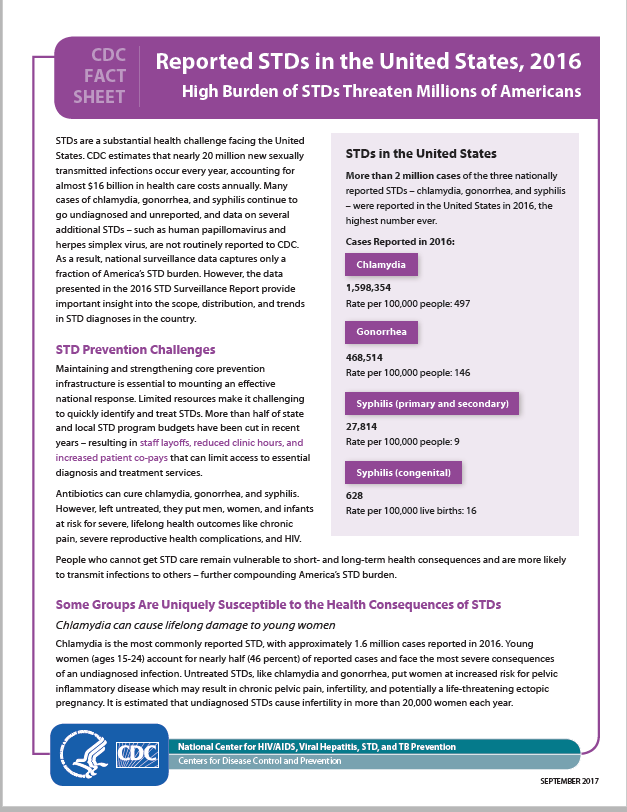
Approximately 20 million new sexually transmitted infections occur each year in the United States. Human papillomavirus (HPV) is thought to be the most common sexually transmitted infection in the U.S. Herpes simplex virus is also one of the most prevalent. Of the three most commonly occurring bacterial STIs, chlamydia, gonorrhea, and syphilis, chlamydia rates are the highest. In 2016, over 1.5 million chlamydial infections were reported to the Centers for Disease Control and Prevention. Reported gonorrhea cases totaled 468, 514. Although the number of primary  and secondary (P&S) syphilis cases is substantially lower than the cases of other infections, in 2016 there were 27,814 P&S cases reported to CDC; and 628 reported cases of congenital syphilis, 41 of which were syphilitic stillbirths.2
and secondary (P&S) syphilis cases is substantially lower than the cases of other infections, in 2016 there were 27,814 P&S cases reported to CDC; and 628 reported cases of congenital syphilis, 41 of which were syphilitic stillbirths.2
 These diseases continue to disproportionately burden American minority populations when compared to Whites. In 2016 considering all race, ethnicity, and age categories, rates of reported gonorrhea cases were highest for Blacks aged 20–24, 15–19, and 25–29 years. The overall rate of chlamydia among Alaska Natives was almost four times the rate of the infection among Whites. And in 2016, the rate of reported P&S syphilis cases among Hispanics was double the rate among Whites. Unfortunately minority race and ethnicity in the U.S. are characteristics often associated with other negative factors affecting health status such as poverty and unemployment. Access to quality STD prevention and treatment services is critical to reducing STD disparities, and many minority persons continue to lack access to health care. For example among all races and ethnicities in the U.S. Hispanics had the lowest rate of health insurance coverage in 2015 at 83.8%.3 Lack of access to quality healthcare is an enduring problem for many Americans. A primary recruitment incentive the researchers used for the Tuskegee Study was the promise of healthcare.
These diseases continue to disproportionately burden American minority populations when compared to Whites. In 2016 considering all race, ethnicity, and age categories, rates of reported gonorrhea cases were highest for Blacks aged 20–24, 15–19, and 25–29 years. The overall rate of chlamydia among Alaska Natives was almost four times the rate of the infection among Whites. And in 2016, the rate of reported P&S syphilis cases among Hispanics was double the rate among Whites. Unfortunately minority race and ethnicity in the U.S. are characteristics often associated with other negative factors affecting health status such as poverty and unemployment. Access to quality STD prevention and treatment services is critical to reducing STD disparities, and many minority persons continue to lack access to health care. For example among all races and ethnicities in the U.S. Hispanics had the lowest rate of health insurance coverage in 2015 at 83.8%.3 Lack of access to quality healthcare is an enduring problem for many Americans. A primary recruitment incentive the researchers used for the Tuskegee Study was the promise of healthcare.
For many of us working to promote health equity, the legacy of the U.S. Public Health Service syphilis study at Tuskegee looms large, and usually negatively.4, 5 This is perhaps especially true for those of us working in STD prevention. However it is important to remember that the infamous study led to the National Research Act of 1974 and institutional review boards that require the protection of human subjects in research, including mandating informed consent.6 And it has also taught us valuable lessons about working effectively and respectfully with communities—all communities—to address public health problems, be they chronic or communicable.
The U.S. STD epidemic has cast a long shadow on the land,7 remaining a persistent threat to the health of Americans, particularly in minority communities. Early on many public health scientists and practitioners understood the impact of social determinants on individual health status.8, 9 For example, to improve access to health care for African Americans with syphilis in five southern states, in 1929 the Rosenwald Fund implemented a treatment program focused on locating people with syphilis and providing treatment. Ironically it was this program, by 1932 under the direction of the federal government, that led to the Tuskegee syphilis study.10
Yes, many challenges remain as we seek to improve the health status of all Americans by preventing and controlling STDs. Yet, instructed by the past and in the spirit of collaboration with partners that include the affected minority communities, the prevention and control of STDs is Mission: Possible. We are committed to treating those at risk for STDs right.
Special thanks to Ms. Valentine for contributing this blog in recognition of STD Awareness Month and as part of the celebration of the 30th anniversary commemoration of CDC’s Office of Minority Health and Health Equity. Our theme for the 30th anniversary commemoration is Mission: Possible. We believe “healthy lives for everyone” is possible and a goal that resonates in public health.
1. Satcher, D. (2000). “National Syphilis Elimination Launch: Nashville, Tennessee, October 7, 1999: Syphilis Elimination: History in the Making-Closing Remarks.” Sexually Transmitted Diseases 27(2): 66-67.
2. Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2016. Atlanta: U.S. Department of Health and Human Services; 2017.
3. Barnett JC, Vornovitsky MS. Current Population Reports, P60-257(RV), Health Insurance Coverage in the United States: 2015. Washington, DC: U.S. Government Printing Office; 2016.
4. Thomas SB, Quinn SC (November 1991). “The Tuskegee Syphilis Study, 1932 to 1972: implications for HIV education and AIDS risk education programs in the black community”. Am J Public Health. 81 (11): 1498–505.
5. Katz, Ralph V.; Green, B. Lee; Kressin, Nancy R.; Kegeles, S. Stephen; Wang, Min Qi; James, Sherman A.; Russell, Stefanie L.; Claudio, Cristina; McCallum, Jan M. (2008-11-01). “The legacy of the Tuskegee Syphilis Study: assessing its impact on willingness to participate in biomedical studies”.
6. Department of Health, Education, and Welfare. THE BELMONT REPORT Office of the Secretary Ethical Principles and Guidelines for the Protection of Human Subjects of Research The National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. April 18, 1979.
7. Parran T. Shadow on the Land: Syphilis. New York, NY: American Social Hygiene Association; 1937
8. Dean HD, Fenton KA. Integrating a Social Determinants of Health Approach into Public Health Practice: A Five-Year Perspective of Actions Implemented by CDC’s National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. Public Health Reports. 2013;128 (Suppl 3):5-11.
9. Avey H, Fuller E, Branscomb J, et al. Using a Health in All Policies Approach to Address Social Determinants of Sexually Transmitted Disease Inequities in the Context of Community Change and Redevelopment. Public Health Reports. 2013;128(Suppl 3):77-86.
10. Jones, James H. (1993). Bad Blood: The Tuskegee Syphilis Experiment. New York: The Free Press. pp. 52–90. ISBN 0-02-916676-4.
Posted on by


