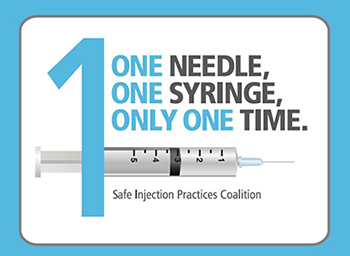
Category: Injection Safety
Multi-Dose Vial Safety Reminders for National Immunization Awareness Month

August is National Immunization Awareness Month, an observance to acknowledge the importance of routine vaccination for people of all ages. Project Firstline wants to ensure that all healthcare workers who give vaccines understand the importance of safe injection practices, and that they use multi-dose vaccine vials safely and correctly. A multi-dose vaccine vial is a Read More >
Posted on by 9 CommentsAsking Your Healthcare Provider the Hard Questions
This blog is a part of a series that CDC launched to highlight the importance of patient safety by providing educational information and simple ways to help people stay informed on public safety topics. Read the blog below, authored by Evelyn McKnight, to learn more about preventing unsafe injection practices. When I was diagnosed with Read More >
Posted on by 4 Comments
