Effective diagnostic processes and patient safety means not having to ask “What if”
Posted on by
“What If” I was seen, heard, and treated like a partner?
Regarded as the greatest English novelist during the Victorian Era, Charles Dickens once said, “It was the best of times, it was the worst of times, it was the age of wisdom, it was the age of foolishness.” Those words never rang truer than with the birth of my son Steven Coffee II—I call him “Deuce” – in late September 2012. In his life, my life would change forever, and the world would be introduced to a living miracle.
When Deuce was born, I felt like a main character in the Disney-Pixar film Inside Out 2. I went through so many emotions: optimism, joy, and the most powerful, love. I cautiously gave my son to the medical staff to run standard newborn screenings and was assured everything would be okay. But, when the medical staff brought Deuce back, my parental intuition told me something was wrong, even though I was assured he was fine.
Deuce wasn’t fine. After several visits to the hospital for additional tests, I received a phone call that again put me back in the movie Inside Out. This call turned my optimism into fear, changed my joy into sadness, and birthed a never-ending anxiety for the safety of my son.
On the call, the provider told me my son had Galactosemia. Several communication challenges made this conversation difficult, but first and foremost, the risks to my newborn son’s health and safety were not adequately explained to me. I later learned this metabolic condition makes him unable to break down galactose in human and animal milk. I continued to listen to the news in fear, which was replaced by panic when the provider told me—the parent without medical training—to go to a larger hospital and tell them about a complex medical condition I could not spell or comprehend. Looking back, I did not have all the information I needed, and I certainly was not equipped to manage a condition so serious on my own.
Feeling as though there was no other option, I recapped the details from the initial call I received about Deuce’s diagnosis as well as my fears and concerns to more doctors at subsequent visits. This time, I was incorrectly told Deuce did not have Galactosemia, only a trait. I was sent home despite my plea for additional testing and answers. My pleas fell on deaf ears in a medical system consumed with shortages of staff and, a diverse and complex patient population. I did not feel heard in that moment or in the almost three weeks that followed as we began our life as new parents. We were caring for our son the best way we knew how, but our harrowing experience was far from over.
As I neared Thanksgiving 2012, traditionally filled with thankfulness and gratitude and regarded as the unofficial start of the holiday shopping season (Black Friday), I was excited. I ventured into the wild of pre-Black Friday sales to get Deuce’s first Christmas toys when I received a phone call that made me drop everything and rush home to take him to the hospital. Deuce had a large swollen mass on his leg that looked concerning. As I entered the hospital anxious and dressed in comfortable clothes from shopping, my concerns were dismissed. Again, my questions went unanswered, and I felt I was not seen. It was as if my comfortable clothes belied the years of military experience, I possess that allowed me to handle high-stress, high-stakes situations. My anxious demeanor muted my military bearing and time spent leading thousands of America’s finest men and women, sons and daughters, in peace and war.
I was regarded as the overreactive new parent who didn’t know about his child. We know now the lump was misdiagnosed as fatty tissue or a swollen lymph node. We were discharged from the hospital and left to disappear into the night without the full knowledge that the mass on Deuce’s leg was a result of his distended stomach, a complication of the original diagnosis of Galactosemia that had gone weeks unconfirmed.
It was just a few days later that we were back in the Pediatric Intensive Care Unit (PICU) when I heard a doctor say, “This is Steven Coffee II, a two-month-old from an outside hospital who has fulminant liver failure secondary to Galactosemia.” It was not until this time that the severity of Deuce’s condition was finally accurately and fully explained to us. Five days later, he became the youngest liver transplant patient in the U.S. at only eight weeks old.
His experience, while unique, is not uncommon. Studies show an estimated 795,000 Americans are harmed or die due to dangerous diseases being misdiagnosed. We must do more to change this reality. The question I asked then is the same one I ask now: What if? What If I was seen as a partner with my son’s healthcare team instead of dismissed? What if my concerns were heard and not dismissed because of bias – seen as a new, anxious father? What if I was seen as a partner in my son’s care? Would my son have needed a liver transplant?
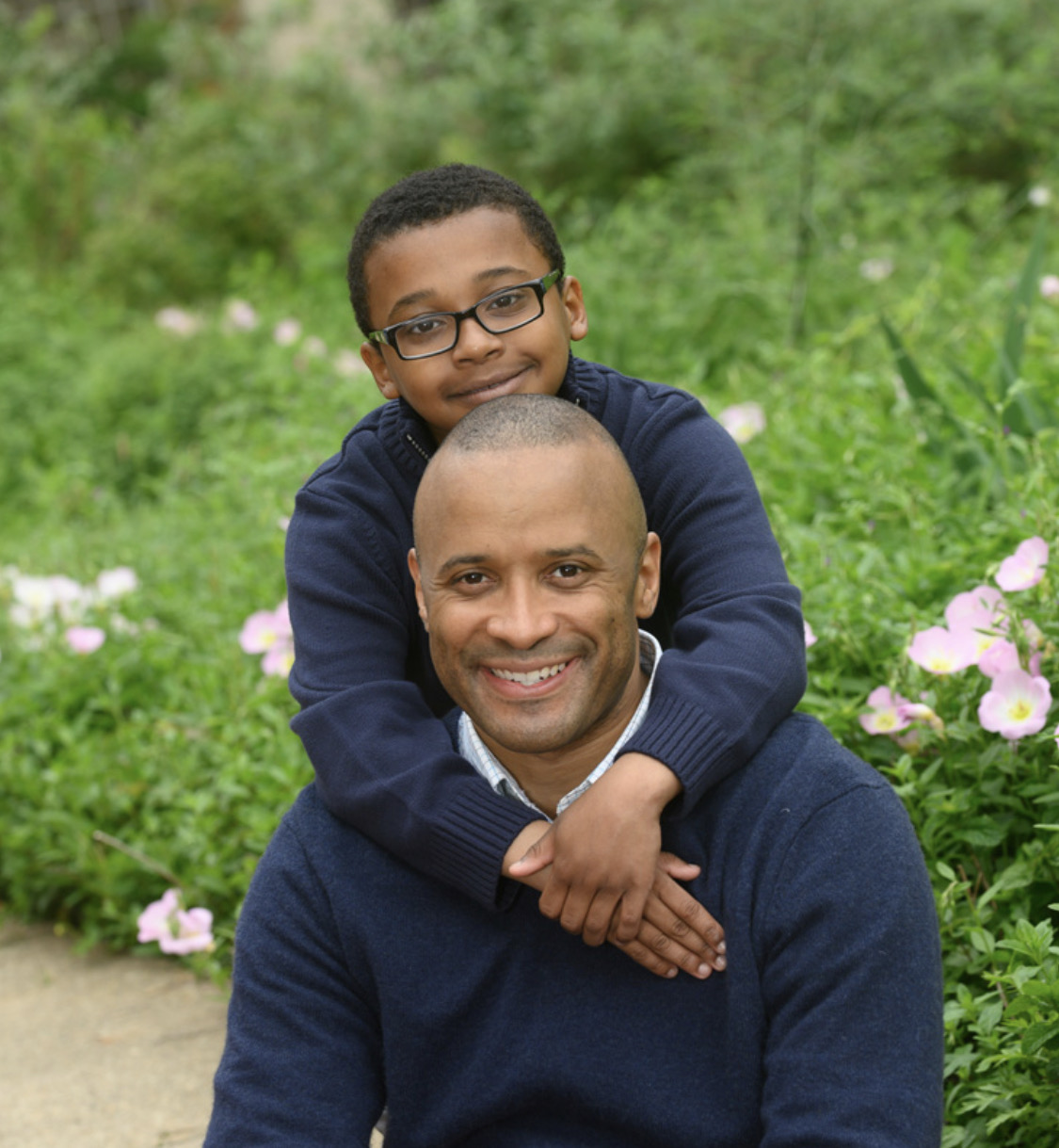
As we approach Deuce’s twelfth birthday, we are beyond grateful and cherish the fact that he is happy and thriving. But as I reflect on those events, my greatest regret is that I doubted myself. When my intuition about patient-provider bias, anchoring in diagnosis, and not being a recognized partner was high, I rationalized, “What if they are right, and I’m just anxious and all those things they say?” As a military officer, I’ve dedicated my life to my country to protect its citizens. As a father, I am dedicated to my son and doing everything in my power to see him thrive and grow, but at that moment, I felt that I could not protect my only son.
My sincere hope is that our story emphasizes the critical importance of clear communication among patients, their families, and their healthcare providers. I don’t want others to feel insecure about asking their care team questions and seeking clarity if they don’t fully understand what the next steps are. Patient safety requires accurate and timely information about a diagnosis and its risks. I want more than anything to protect other people’s sons, daughters, mothers, fathers, sisters, and brothers from having to ask, “What if?”
For information on what CDC is doing to help improve patient safety, see the Core Elements of Hospital Diagnostic Excellence.
Col. Steven L. Coffee is a devoted father and advocate for patient safety, driven by his personal experience of raising a son with Galactosemia. With a passion for effective diagnostic processes, Col. Coffee leverages his unique perspective to educate healthcare professionals and the public. His commitment to improving medical practices stems from firsthand challenges, and he is dedicated to ensuring that no family has to wonder “What if.” Through his work, he aims to inspire change and enhance the reliability of diagnostic procedures, ultimately safeguarding patient health and well-being. He currently serves as a Military Deputy to the Deputy Assistant Secretary, overseeing strategic plans and policies for 700,000 Air and Space Force personnel. He specializes in compensation, education, training, and personnel policy and brings a wealth of knowledge to his role.
Posted on by

