CDC Supports Microbiome Science to Advance Infection Prevention, Clinical Care, and Public Health
Posted on by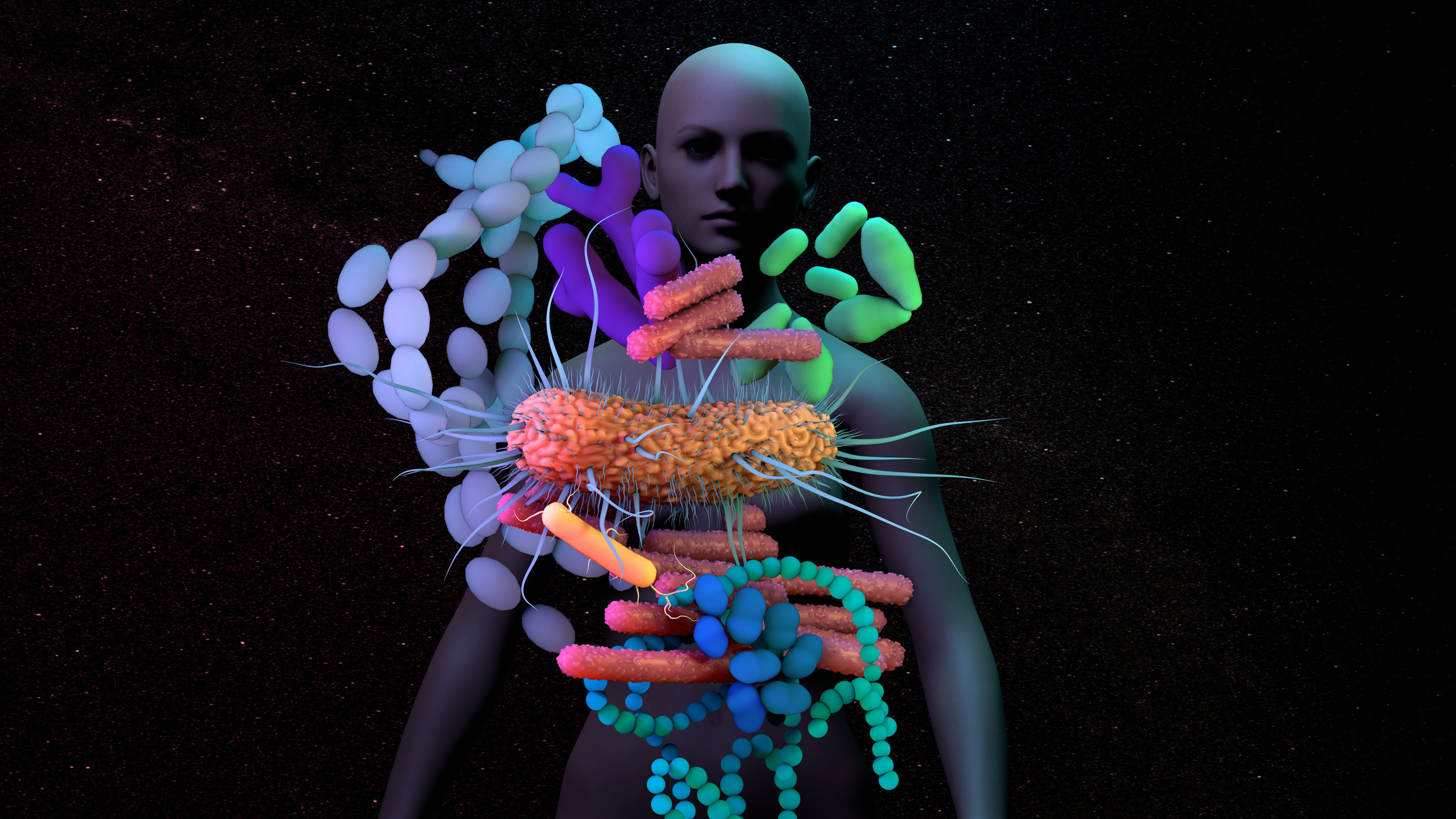
Infectious disease experts at the U.S. Centers for Disease Control and Prevention (CDC) and the National Institutes of Health (NIH) recently co-edited a special issue of the Journal of Infectious Diseases (JID) featuring 16 review articles on innovative research of the human microbiome, which is the community of naturally occurring microorganisms in and on our bodies. This work represents ongoing engagement and financial support from CDC’s Antibiotic Resistance (AR) Solutions Initiative to leverage the microbiome for new ways to prevent antibiotic-resistant infections.
Released on June 15, 2021, the journal supplement highlights the significant promise the human microbiome holds for addressing public health challenges like antibiotic resistance (AR)—one of the greatest modern public health threats—with topic areas ranging from sepsis, Clostridioides difficile (C. difficile) and necrotizing enterocolitis, to the vaginal, gut, and lung microbiomes. The authors highlight innovations in microbiome research that may protect people from infectious diseases and antibiotic-resistant microorganisms, such as microbiome indices measuring the health status of a patient’s microbiome, targeting resistant microbes, and live biotherapeutics.
CDC is committed to furthering microbiome science for public health. However, we have much more to learn as current microbiome research and discoveries only scratch the surface. In addition to significant funding directed by CDC and NIH towards microbiome-related research, there is a pressing need for further clinical, translational, and infection prevention research to move beyond understanding and into implementation of prevention and mitigation strategies in the clinical and public health fields. For public health specifically, CDC experts see opportunities for microbiome-based solutions to restore gut health (where many opportunistic pathogens reside), predict disease severity, and mitigate or cure infections.
Microbiome-based therapies are an opportunity to restore gut health without increasing antibiotic resistance.
Research featured in the supplement highlights the role the gut microbiome plays as a barrier to colonization (when pathogens survive and multiply without causing infection) by pathogenic, and often resistant, microbes. Researchers discuss the opportunity to manipulate the gut microbiome as a therapeutic for the costly and preventable healthcare-associated infection, C. difficile (Pike and Theriot). In addition to pathogens, the gut microbiome can house a wide variety of AR genes and plasmids. This reservoir of resistance genes can be shared with other microbes in the gut but also holds promise for future diagnostics and treatments. Examples of clinical application of the plasmids include metagenomic sequencing in outbreak tracing and personalized medicine, such as identifying drug-microbiome interactions to improve patient outcomes (Anthony et al.). The interactions between microbial communities and human hosts can impact and drive disease acuity and progression. In “Microbiome data enhances predictive models of lung function in people with cystic fibrosis”, Zhao et al. used sputum microbiome data from 77 cystic fibrosis (CF) patients to examine the relationship between microbial communities present in the patients’ lungs and their health outcomes.
Microbiomes across the body can impact disease severity.
Unique microbiomes with varying bacterial compositions are located across the human body from the gut to the vagina to the skin. The microbes within microbiomes are reflective of physiology, environmental exposures, diets, immune system changes, antibiotic exposure and more. In the issue, Pettigrew et al. discuss an ecological model of pneumonia as a disease “that exists on a continuum of microbiota abundance, diversity, and composition with a range of corresponding immune states.” Although unique, specialized human anatomical sites that house microbiomes do not exist independently of one another. For example, the gut and oral cavity are potential sources of pathogens affecting the lungs and must be considered holistically to inform prevention and treatment plans. Two studies (Miller et al. and Thänert et al.) explore the influence and role of the microbiome in the pathogenesis of two diseases (sepsis and necrotizing enterocolitis, respectively) hallmarked by systemic inflammation and variable sources of infection, as well as the possibility of leveraging the microbiome to improve patient outcomes.
Microbiomes hold promise to mitigate or cure disease.
In recent years, fecal microbiota transplantation (FMT) has garnered increased attention from the media and public as a treatment for a wide range of conditions. Gerardin et al. summarize how FMT can improve C. difficile (and other) infection outcomes and prevent reoccurrence through decolonization. With hundreds of clinical trials involving FMT underway and many microbiome drugs in development, the opportunity to transform patient care and improve patient outcomes is indicative of the critical nature of microbiome science.
Demonstrating the depth and breadth of microbiome research, the microbiome special issue shines a spotlight on the many potential avenues to improve health outcomes. This supplement discusses translation of basic science advancing our ability to prevent, diagnose, and treat antimicrobial-resistant and other infections, but there remains a need to move beyond correlation between disease and microbiome state to actually elucidating the microbiome’s role in the causal pathway to disease. As the only compilation to date of cutting-edge human microbiome research focused on antibiotic resistance and infectious diseases, this supplement serves as a unique compendium and authoritative source of innovations in microbiome.
Many researchers featured in this supplement have had work previously funded by CDC’s AR Solutions initiative. Learn more about CDC’s innovate projects to combat antibiotic resistance.
Melia Haile, MPH, CHES, is a Public Health Advisor for the Division of Healthcare Quality Promotion, within the National Center for Emerging and Zoonotic Infectious Diseases.
Alison Laufer Halpin, PhD, is an Associate Director of the Office of Scientific Innovation and Integration in the Clinical and Environmental Microbiology Branch of the Division of Healthcare Quality Promotion within the National Center for Emerging and Zoonotic Infectious Diseases. Halpin is also a Commander in the U.S. Public Health Service.
Clifford McDonald, MD, is an Associate Director for Science and Integrity, in the Division of Healthcare Quality Promotion, within the National Center for Emerging and Zoonotic Infectious Diseases.
Chris Elkins, PhD, Chief in the Clinical and Environmental Microbiology Branch, of the Division of Healthcare Quality Promotion in the National Center for Emerging and Zoonotic Infectious Diseases.
Posted on by

