Wadsworth Center Bacteriology Laboratory
Posted on by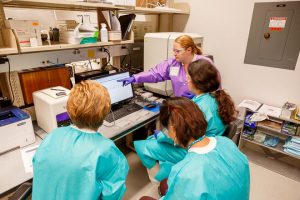
Kimberlee A. Musser, Ph.D.
Chief, Bacterial Diseases
Wadsworth Center, NYSDOH
Souvenirs: What did you bring home from your last trip to the hospital?
The stuff we carry around says a lot about us. If I were to dump my purse right now, you’d find a shell from my last trip to the ocean, a garnet from a hike up north, and a penny pressed from an amusement park. Bacteria tell us a lot about themselves from the stuff (genes) they carry around as well. Just as you can tell where I’ve been from the contents of my purse, scientists can tell where bacteria have been from the contents of their genes.
You see, they pick up antibiotic resistance genes from each other, which doesn’t sound like a bad thing until they get a big collection going, and then they’re resistant to just about every antibiotic we have against them. That’s why healthcare-associated infections can be so serious. These bacteria are with a lot of other bacteria and can become resistant to many antibiotics, making them very difficult to fight. One such organism we call CRAB, or carbapenem-resistant Acinetobacter baumannii, is resistant to just about all the antibiotics currently used to treat it.
As part of CDC’s Antibiotic Resistance Lab Network, the Wadsworth Center Bacteriology Laboratory in Albany, NY, tested 14 patient specimens from an outbreak at a large hospital in our region. The first tests performed (called MALDI-TOF MS) were to confirm which organism we were dealing with. Once we confirmed it was Acinetobacter baumannii, we looked in the purse and found a bunch of souvenirs!
Some of the 14 specimens had apparently visited the same attractions and were resistant to the same set of antibiotics. The remaining specimens were resistant to a different set of antibiotics. We were able to determine this with a test we developed in our laboratory (real-time PCR). We didn’t stop there. We confirmed these resistance patterns by sequencing the entire genome of these bacteria (another test called whole genome sequencing or WGS). This testing was possible only through the support of CDC antibiotic resistance investments through the Epidemiology and Laboratory Capacity for Infectious Diseases (ELC) Cooperative Agreement, which provided for the staff who developed and performed the tests, as well as the testing materials and instrumentation. These are very specialized tests not performed at most laboratories, or even public health laboratories, so support of this laboratory to perform this kind of testing is critical.
Why does this testing matter? Certainly, it matters to the people who are sick. Instead of being treated with one antibiotic after another, trying to find one that works, we can quickly say which antibiotics won’t work and, most importantly, which will.
It is also invaluable to infection control specialists and epidemiologists who are trying to track down how the infection is spreading and what the source is in order to stop the outbreak or spread of these bacteria. It is also important to the public who can go to the hospital for procedures, or to visit, or to work, without fear of becoming ill. Testing performed from this one outbreak demonstrates that the algorithm, or specific tests that we are using, is effective at rapidly identifying which organism is causing the outbreak and exactly which antibiotics to which the bacteria is resistant and sensitive.
Just as I didn’t know what surprises my purse held until I emptied it, not until the specialized testing, possible only through the support of CDC, did we know about many of the surprises held by the genes of the resistant organisms. What we do know is that we still have much to learn about these crafty bacteria, how they spread and cause disease, and how successful infection control strategies can be in the fight against antimicrobial resistance.
Posted on by

