Do We Need to Challenge Respirator Filters With Biological Aerosols?
Posted on by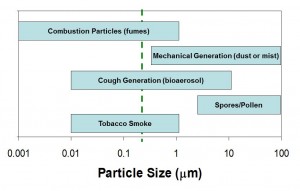
The purpose of this NIOSH Science Blog is to explain what is currently known about an important aspect of respirator filtration. For decades, respirator researchers have been asked whether filters need to be tested with aerosols similar to those encountered in the environment (Figure 1). Common sense suggests that viruses or bacteria are collected differently from engineered nanoparticles, silica dusts, oil mists or other types of workplace aerosols.
But this may not be the case. Why is that?
Particle capture or collection by a respirator filter depends on the physical characteristics of the particle – shape, size and density.(1, 2) Whether the particle is “living” or “infectious” plays no role in how well it will be collected by a filter.(3) Once a particle is collected it will remain attached by electrostatic and van der Waals’ forces and will not easily migrate.(4) Biological organisms have no capacity for moving on their own through a filter.(5) Particles are very hard to remove from a filter once they are collected – the forces keeping a particle attached to the filter are surprisingly strong.(2, 4-6)
Researchers have developed an understanding of how different test conditions affect respirator filtration efficiency.(2, 4, 7-9) This information can be exploited to create most rigorous or “worst case” type conditions for testing. Important features of a “worst case” filter performance test include:
- The test aerosol should include particles at or near the most penetrating particle size range.(2, 8)
- The test air flow should be near the highest level encountered during heavy work, because higher air flow leads to more particles getting through the filter.(2, 8, 10) Tests that do not specify a high air flow or allow selection from a range of air flows can be easily manipulated to produce results that suggest a filter will be more effective than they will actually perform.(11, 12).
- The test aerosol should be charge neutralized (have an equal distribution of positively and negatively charged particles), because charge neutralization has been shown to lower the filter collection of particles.(9) Test protocols that do not require charge neutralization of the challenge aerosol may suggest that filters will perform with higher efficiency than may be the case in the “real world.”
- The detection method should be able to measure particles in the most penetrating particle size range with high sensitivity and precision. Direct reading instruments that measure how particles scatter light have greater sensitivity and precision than bioassays that require viable viruses or bacteria, multiple dilutions, specific growth media, temperature-controlled growth conditions and well-trained technicians to count colonies.(13)
The test conditions used by NIOSH in 42 Code of Federal Regulations Part 84 for respirator certification testing of air purifying respirators are believed to represent near “worst case” conditions for all types of workplaces.(7, 14) (See: NIOSH Science Blog, N95 Respirators and Surgical Masks, Section on “How do filters collect particles” and Respiratory Protection for Workers Handling Engineered Nanoparticles. This ensures that filters in NIOSH certified respirators will collect all types of workplace aerosols – including emerging hazards such as airborne infectious organisms (15) and engineered nanoparticles (7) – with very high efficiency.
What do these data mean for respirator filter testing?
The literature cited in this Science Blog suggest that it is not necessary to test a respirator filter with a biological aerosol, but rather to focus on “worse-case” type test conditions. When properly selected and used, respirators tested using these types of filter tests should provide expected levels of protection against all types of workplace aerosols.
A federal register notice was published on March 14, 2014 to solicit additional input on several topics, including this issue. Specifically, NIOSH is seeking information and comments to assess whether NIOSH should consider additional filter test methods to enhance existing requirements. Are there any important developments in aerosol science or key scientific data that would better inform NIOSH on the filtration of biological aerosols? Comments may be submitted to NIOSH Docket #272 by April 30, 2014 through this site: http://www.regulations.gov/#!docketDetail;D=CDC-2014-0005. Comments to this NIOSH Science blog made by April 30, 2014 will be added to NIOSH Docket #272.
Lisa M. Brosseau, ScD, CIH and Ronald Shaffer, PhD
Dr. Brosseau is a Professor in the Division of Environmental and Occupational Health Sciences at the University of Illinois at Chicago School of Public Health.
Dr. Shaffer is Chief of Technology Research Branch at NIOSH’s National Personal Protective Technology Laboratory.
References
1 McCullough, N., L. Brosseau, and D. Vesley: Collection of three bacterial aerosols by respirator and surgical mask filters under varying conditions of flow and relative humidity. Annals of occupational hygiene 41(6): 677-690 (1997).
2 Hofacre, K.C., A.W. Richardson, J.P. Eshbaugh, and P.D. Gardner: “Respirator filter efficiency testing against particulate and biological aerosols under moderate to high flow rates.” Edgewood Chemical Biological Center ECBC-CR-085, 2006. [Available at NIOSH Docket #272]
3 Harnish, D., B. Heimbuch, M. Husband, A. Lumley, K. Kinney, R. Shaffer et al.: Challenge of N95 Filtering Facepiece Respirators with Viable H1N1 Influenza Aerosols. Infection control and hospital epidemiology: the official journal of the Society of Hospital Epidemiologists of America 34(5): 494 (2013).
4 Hinds, W.C.: Aerosol technology: properties, behavior, and measurement of airborne particles: John Wiley & Sons, 2012.
5 Fisher, E.M., A.W. Richardson, S.D. Harpest, K.C. Hofacre, and R.E. Shaffer: Reaerosolization of MS2 bacteriophage from an N95 filtering facepiece respirator by simulated coughing. Annals of occupational hygiene 56(3): 315-325 (2012).
6 Kennedy, N.J., and W.C. Hinds: Release of simulated anthrax particles from disposable respirators. J Occup Environ Hyg 1(1): 7-10 (2004).
7 Shaffer, R.E., and S. Rengasamy: Respiratory protection against airborne nanoparticles: a review. Journal of nanoparticle research 11(7): 1661-1672 (2009).
8 Stevens, G.A., and E.S. Moyer: “Worst case” aerosol testing parameters: I. Sodium chloride and dioctyl phthalate aerosol filter efficiency as a function of particle size and flow rate. The American Industrial Hygiene Association Journal 50(5): 257-264 (1989).
9 Moyer, E.S., and G.A. Stevens: “Worst-Case” Aerosol Testing Parameters: III. Initial Penetration of Charged and Neutralized Lead Fume and Silica Dust Aerosols through Clean, Unloaded Respirator Filters. The American Industrial Hygiene Association Journal 50(5): 271-274 (1989).
10 Eshbaugh, J.P., P.D. Gardner, A.W. Richardson, and K.C. Hofacre: N95 and P100 respirator filter efficiency under high constant and cyclic flow. Journal of Occupational and Environmental Hygiene 6(1): 52-61 (2008).
11 Oberg, T., and L.M. Brosseau: Surgical mask filter and fit performance. American journal of infection control 36(4): 276-282 (2008).
12 Rengasamy, S., A. Miller, B.C. Eimer, and R.E. Shaffer: Filtration performance of FDA-cleared surgical masks. Journal of the International Society for Respiratory Protection 26(1): 54 (2009).
13 Brosseau, L.M., N.V. McCullough, and D. Vesley: Mycobacterial aerosol collection efficiency of respirator and surgical mask filters under varying conditions of flow and humidity. Applied occupational and environmental hygiene 12(6): 435-445 (1997).
14 NIOSH: “NIOSH Guide to the Selection and Use of Particulate Respirators Certified Under 42 CFR 84.” [Online] Available at http://www.cdc.gov/niosh/docs/96-101/, (1996).
15 Janssen, L., H. Ettinger, S. Graham, R. Shaffer, and Z. Zhuang: Commentary: The Use of Respirators to Reduce Inhalation of Airborne Biological Agents. Journal of Occupational and Environmental Hygiene 10(8): D97-D103 (2013).
16 Zayas, G., M.C. Chiang, E. Wong, F. MacDonald, C.F. Lange, A. Senthilselvan et al.: Cough aerosol in healthy participants: fundamental knowledge to optimize droplet-spread infectious respiratory disease management. BMC pulmonary medicine 12(1): 11 (2012).
17 Baron, P.: “Generation and Behavior of Airborne Particles (Aerosols).” [Online] Available at http://www.cdc.gov/niosh/topics/aerosols/pdfs/Aerosol_101.pdf, (2010).
18 NIEH: “Particles: Size Makes All the Difference.” [Online] Available at http://www.niehs.nih.gov/health/assets/docs_a_e/ehp_student_edition_lesson_particles_size_makes_all_the_difference.pdf, (2006).
8 comments on “Do We Need to Challenge Respirator Filters With Biological Aerosols?”
Comments listed below are posted by individuals not associated with CDC, unless otherwise stated. These comments do not represent the official views of CDC, and CDC does not guarantee that any information posted by individuals on this site is correct, and disclaims any liability for any loss or damage resulting from reliance on any such information. Read more about our comment policy ».
We like your respirator filtration blog explanation. You explain as very well. We get valuable information also a valuable explanation from you. Thank you.
angelina from
All investigations and efforts that make NIOSH to do reliable breathing filters will be valuable to protect the health of workers subject to the danger of pollutants and harmful particles. The carcinogenic consequences of various industrial substances have already been demonstrated and reliable protection for workers is an important objective that NIOSH should pursue.
In March 2014 NIOSH issued a request for information and comment on “Respiratory Protective Devices Used in Healthcare.” Comments were requested in response to four topics. Public comments were received, compiled, and a NIOSH response formulated. The Federal Register Notice, Comments, and NIOSH response are available on http://www.regulations.gov Search CDC-2014-0005
excellent information. must read the contents.
Especially for biological hazards, faceseal leakage is as or even more significant than is filter penetration.
A number of years ago NIOSH proposed criteria to measure for Total Inward Leakage, rather than just
filtration, but for unknown reasons, NIOSH dropped this proposal a few years later. it needs be noted
that an N95 can have a TOTAL inward leakage of upto 10%, which is way to high and dangerous, and totally
inadequate for exposure to aerosolized pathogens.
Excellent Point Dr. Lantos. Would like to also see study with respect to enhanced eficacy when using first aid tapes to seal the respirator to the HCP’s face, including clean shaven and after one or two day stubble. Long hours in the ICU, ER, etcetera as we all know can affect the facial interface. Thank you.
Will a properly sized and fitted NIOSH N95 Respirator filter particles 0.13 microns or smaller in diameter? What are the Upper/Lower limits of the NIOSH N95 Respirator? If possible please provide documentation/links.
HJ, HMC USN
A NIOSH-approved N95 filtering facepiece respirator (FFR) is a type of respirator which removes particles from the air that are breathed through it. These respirators filter out at least 95% of very small (0.3 micron) particles. NIOSH-approved N95 FFRs can efficiently capture 0.1 um size particles and are capable of filtering out all types of particles, including bacteria and viruses. Inert particles as well as bacterial and viral particles are captured by the same mechanisms (NIOSH, 2018; Qian et al., 1998). Whether the particle is “living” or “infectious” plays no role in how well a filter will collect it (Harnish et al., 2013). The minimum filtration efficiency of an N95 is 95% and the maximum is up to 99.97%.
References:
NIOSH (2018) A Particle is a Particle (video). https://www.cdc.gov/niosh/npptl/particle.html.
Qian et al. (1998) Amer Ind Hyg Assoc J. 59:128-132
Harnish et al. (2013) Infect. Control Hosp. Epidemiol. 34, 494-499.